With American hospitals facing a dire shortage of nurses amid a slogging pandemic, many are looking abroad for health care workers. And it could be just in time.
There’s an unusually high number of green cards available this year for foreign professionals, including nurses, who want to move to the United States — twice as many as just a few years ago. That’s because U.S. consulates shut down during the coronavirus pandemic weren’t issuing visas to relatives of American citizens, and, by law, these unused slots now get transferred to eligible workers.
Amy L. Erlbacher-Anderson, an immigration attorney in Omaha, Nebraska, said she has seen more demand for foreign nurses in two years than the rest of her 18-year career. And this year, she said, it’s more likely they’ll get approved to come, so long as U.S. consular offices can process all the applications.
“We have double the number of visas we’ve had available for decades,” she said. “That is kind of temporarily creating a very open situation.”
 U.S. hospitals are struggling with a shortage of nurses that worsened as pandemic burnout led many to retire or leave their jobs. Meanwhile, coronavirus cases continue to rise and fall, placing tremendous pressure on the health care system. In California alone, there’s an estimated gap of 40,000 nurses, or 14% of the workforce, according to a recent report by the University of California, San Francisco.
U.S. hospitals are struggling with a shortage of nurses that worsened as pandemic burnout led many to retire or leave their jobs. Meanwhile, coronavirus cases continue to rise and fall, placing tremendous pressure on the health care system. In California alone, there’s an estimated gap of 40,000 nurses, or 14% of the workforce, according to a recent report by the University of California, San Francisco.
Hospitals are filling the gap by hiring traveling nurses, but that can be expensive. And hospital administrators say not enough nurses are graduating from U.S. schools each year to meet the demand.
Some hospitals have long brought nurses from the Philippines, Jamaica and other English-speaking countries, and more are now following suit. And both longtime recruiters and newcomers are trying to take advantage of the green card windfall before the fiscal year ends in September.
The U.S. typically offers at least 140,000 green cards each year to people moving to the country permanently for certain professional jobs, including nursing. Most are issued to people who are already living in the United States on temporary visas, though some go to workers overseas. This year, 280,000 of these green cards are available, and recruiters hope some of the extras can be snapped up by nurses seeking to work in pandemic-weary hospitals in the United States.
The Biden administration, which has made moves to reverse Trump-era policies restricting legal immigration, has taken some steps to try to help foreign health care workers so they can assist with the pandemic. U.S. Citizenship and Immigration Services said it would speed the renewal of work permits for health care workers, which could help keep some foreign citizens already in the United States on the job. The State Department told consulates last year to prioritize applications for workers at facilities that are responding to the pandemic, an agency official said.
Faith Akinmade, a 22-year-old nurse from Nigeria, is among those hoping for a quick solution. After completing college in the U.S., Akinmade has been working as an ICU nurse for University of Louisville Hospital in Kentucky. But her work permit is set to expire in March. She said she needs it renewed, or her green card approved, to stay on the job.
“At this point and time, I just feel like I have faith that at the end of March something is going to show up to continue to work,” Akinmade said. She said the issue affects many of her international colleagues as well as domestic ones, who may be pressed to take on shifts for colleagues if their immigration paperwork doesn’t come through.
Dr. Roxie Wells, president of Cape Fear Valley Hoke Hospital in Raeford, North Carolina, said she started trying to bring over foreign nurses before the pandemic, but it wasn’t until last year that these recruits started getting consular interviews in larger numbers. So far, about 150 were approved to come work, but Wells said they’re still waiting on another 75.
“Obviously it has become more necessary during the pandemic,” she said. “The 150, if we didn’t have them, we would be in a precarious situation.”
The surge in the omicron variant in the United States has made the strained staffing situation even more apparent in hospitals as health care workers, like so many others, have been sickened by the highly contagious virus and sidelined from work at a time when more patients are coming in.
Sinead Carbery, president of International Nurse Staffing Solutions for AMN Healthcare, said the demand for international nurses has risen between 300% and 400% since the pandemic began. The number of nurses that can be brought into the United States even with the additional green cards won’t be enough to meet demand, and many more recruiters are now seeking to hire nurses overseas because there are immigrant visas available, she said.
“This is a window of opportunity,” she said. “Because everything is flowing so well, there’s a lot of competition for that talent.”
National Nurses United, a union representing 175,000 registered nurses, said more scrutiny should be given to international recruitment to ensure foreign nurses aren’t brought in and subjected to unsafe working conditions. The union contends hospitals drove away U.S. nurses by keeping staffing levels so low — and this was well before concerns arose about worker safety and protections during the COVID-19 pandemic.
Michelle Mahon, the union’s assistant director of nursing practice, said many foreign nurses sign yearslong contracts with employers, which can make it hard for them to speak up about labor or patient safety concerns. She said hospitals that saw nurses quit during the pandemic are turning to an overseas workforce to replace them.
“This kind of dynamic is particularly attractive right now to employers who have not made any of the changes necessary to ensure patient and nursing safety during this COVID-19 pandemic,” Mahon said. “Instead of them addressing the actual problem, they want to go and pivot to this other really fake solution.”
Hospital administrators, however, contend there simply aren’t enough U.S.-trained nurses to go around. Patty Jeffrey, president of the American Association of International Healthcare Recruitment, said the United States should expand nursing education programs to train more nurses domestically, as well as let more nurses come in from overseas. But she acknowledged bringing in a much larger number of nurses would require legislation.
“The calls are every day ringing off the hook: We need 100, we need 200, we need all these nurses,” Jeffrey said.
Jorge Almeida Neri, a 26-year-old nurse from Portugal, arrived in the United States late last year, though he began the process before the pandemic. He said a required international nursing exam was delayed due to the virus and it took four months to get a consular interview, though other international nurses he’s met waited much longer. He interviewed for his current job at a Virginia hospital, which he got through a staffing agency, about a year ago.
“After getting everything certified, the immigration process started, and I was like, ‘Oh, this is going to be quick.’ I was wrong,” he said.
Almeida Neri said many Portuguese nurses seek work overseas since wages are low, though many go elsewhere in Europe, which doesn’t take as long as the United States.
Despite the demand, there’s no guarantee hospitals will in fact snap up more visas. Greg Siskind, an immigration attorney, said U.S. consular offices aren’t required to issue visas solely because they’re available, and are hampered by limits on remote work and video interviews. He said most employment-based green cards tend to go to professionals already in the United States, not overseas, though more could be done to speed these up, too.
“Under their current policies, if they don’t make any changes, it is going to be hard,” he said of the likelihood the U.S. government will issue all the available visas, “but there’s a lot of things they could do.”



 In adults, small amounts can quickly cause dangerously low blood pressure, dizziness, fainting, or even heart attacks or strokes, said Dr. Kelly Johnson-Arbor, Co-Medical Director of the National Capital Poison Center in Washington, D.C. Higher doses can be fatal, she and her colleagues wrote in The American Journal of Emergency Medicine. Sodium azide levels in COVID-19 rapid test kits are not always high enough to cause low blood pressure in adults, and the iHealth kits being sent out by the U.S. government do not contain any sodium azide at all, Johnson-Arbor said. “However… since children are typically much smaller than adults, they are at a higher risk of experiencing poisonous effects after swallowing any amount,” she said.
In adults, small amounts can quickly cause dangerously low blood pressure, dizziness, fainting, or even heart attacks or strokes, said Dr. Kelly Johnson-Arbor, Co-Medical Director of the National Capital Poison Center in Washington, D.C. Higher doses can be fatal, she and her colleagues wrote in The American Journal of Emergency Medicine. Sodium azide levels in COVID-19 rapid test kits are not always high enough to cause low blood pressure in adults, and the iHealth kits being sent out by the U.S. government do not contain any sodium azide at all, Johnson-Arbor said. “However… since children are typically much smaller than adults, they are at a higher risk of experiencing poisonous effects after swallowing any amount,” she said.
 “Our COVID-19 vaccine has been administered to hundreds of millions of people around the world, protecting people from COVID-19 infection, hospitalization and death,” Moderna CEO Stéphane Bancel said in a statement. “The totality of real-world data and the full [approval] for Spikevax in the United States reaffirms the importance of vaccination against this virus. This is a momentous milestone in Moderna’s history as it is our first product to achieve licensure in the U.S.”
“Our COVID-19 vaccine has been administered to hundreds of millions of people around the world, protecting people from COVID-19 infection, hospitalization and death,” Moderna CEO Stéphane Bancel said in a statement. “The totality of real-world data and the full [approval] for Spikevax in the United States reaffirms the importance of vaccination against this virus. This is a momentous milestone in Moderna’s history as it is our first product to achieve licensure in the U.S.”
 “We write today urging you to take legislative action as swiftly as possible to lower drug prices,” the Democrats, many of whom represent competitive seats,
“We write today urging you to take legislative action as swiftly as possible to lower drug prices,” the Democrats, many of whom represent competitive seats, 
 The governors had met earlier with
The governors had met earlier with 

 They say the book is for anyone who is looking to reset their food habits which are in sync with their own body, mind and health.
They say the book is for anyone who is looking to reset their food habits which are in sync with their own body, mind and health.

 “We anticipate that there will be a period of quiet before Covid-19 may come back towards the end of the year, but not necessarily the pandemic coming back,” Kluge said. Top US scientist Anthony Fauci expressed similar optimism on Sunday.
“We anticipate that there will be a period of quiet before Covid-19 may come back towards the end of the year, but not necessarily the pandemic coming back,” Kluge said. Top US scientist Anthony Fauci expressed similar optimism on Sunday.
 The worst-case scenario is the emergence of a still-more dangerous variant, he said. He said this possibility is more reason for people to get vaccinated and receive booster shots, and to make testing and medical treatment more widely available.
The worst-case scenario is the emergence of a still-more dangerous variant, he said. He said this possibility is more reason for people to get vaccinated and receive booster shots, and to make testing and medical treatment more widely available.

 During the much anticipated CEOs Forum, a panel of healthcare experts, health industry leaders, opinion makers, and community organizers discussed the significance of promoting Preventive healthcare in India.
During the much anticipated CEOs Forum, a panel of healthcare experts, health industry leaders, opinion makers, and community organizers discussed the significance of promoting Preventive healthcare in India. Analyzing and assimilating the diverse and expert views expressed by the renowned speakers at the CEO Forum regarding the current state of healthcare in India, the CEO Forum provided a great stage to interact with a varied and distinct group of individuals and corporations, and comprehend the complex dynamics of the commerce of health care enterprise.
Analyzing and assimilating the diverse and expert views expressed by the renowned speakers at the CEO Forum regarding the current state of healthcare in India, the CEO Forum provided a great stage to interact with a varied and distinct group of individuals and corporations, and comprehend the complex dynamics of the commerce of health care enterprise. Urging the Government of India to encourage private hospitals and insurance companies to provide Annual Physical exams, or Telehealth visits at an affordable cost to patients, the CEO Forum members stated, “many routine lab tests, vaccinations, blood pressure checks, and some cancer screenings like self-breast examination can be done remotely and even at patients’ homes with the help of Asha
Urging the Government of India to encourage private hospitals and insurance companies to provide Annual Physical exams, or Telehealth visits at an affordable cost to patients, the CEO Forum members stated, “many routine lab tests, vaccinations, blood pressure checks, and some cancer screenings like self-breast examination can be done remotely and even at patients’ homes with the help of Asha 
 Thirteen rounds were conducted on the DD National channel between 7 and 7:30 am. Many leading Yoga gurus and institutes like the Indian Yoga Association, National Yoga Sports Federation participated. In his address, Sonowal highlighted the advantages, “Scientifically, the Surya Namaskar has been known to develop immunity and improve vitality, which is significant to our health during the pandemic conditions.”
Thirteen rounds were conducted on the DD National channel between 7 and 7:30 am. Many leading Yoga gurus and institutes like the Indian Yoga Association, National Yoga Sports Federation participated. In his address, Sonowal highlighted the advantages, “Scientifically, the Surya Namaskar has been known to develop immunity and improve vitality, which is significant to our health during the pandemic conditions.”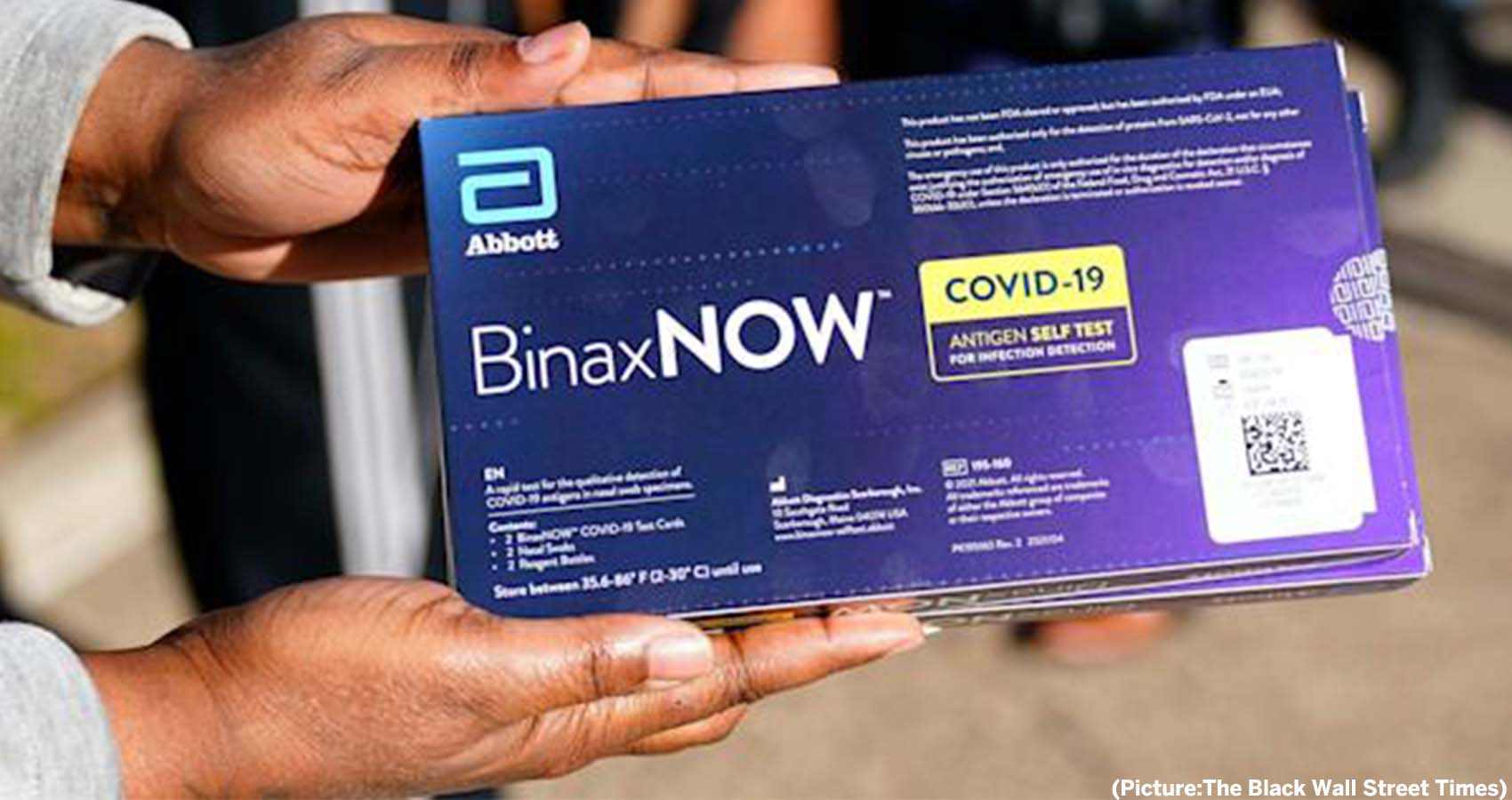
 Public health experts and the Centers for Disease Control and Prevention recommend that Americans use at-home tests if they begin to have symptoms, at least five days after coming in close contact with someone who has COVID-19, or are gathering indoors with a group of people who are at risk of severe disease or unvaccinated.
Public health experts and the Centers for Disease Control and Prevention recommend that Americans use at-home tests if they begin to have symptoms, at least five days after coming in close contact with someone who has COVID-19, or are gathering indoors with a group of people who are at risk of severe disease or unvaccinated.
 “Although Congress has indisputably given OSHA the power to regulate occupational dangers, it has not given that agency the power to regulate public health more broadly. Requiring the vaccination of 84 million Americans, selected simply because they work for employers with more than 100 employees, certainly falls in the latter category,” the unsigned opinion in the businesses case says.
“Although Congress has indisputably given OSHA the power to regulate occupational dangers, it has not given that agency the power to regulate public health more broadly. Requiring the vaccination of 84 million Americans, selected simply because they work for employers with more than 100 employees, certainly falls in the latter category,” the unsigned opinion in the businesses case says.
 “The study sought to quantify the frequency of and risk factors for severe outcomes in children with COVID-19,” says study co-lead
“The study sought to quantify the frequency of and risk factors for severe outcomes in children with COVID-19,” says study co-lead 

 In continuation of its efforts, during the recently concluded Global Healthcare Summit in Hyderabad, AAPI donated immunoanalyzer at AIIMS, Bibinagar, Telangana, which does hundreds of tests every day. This is part of Covid relief efforts AAPI has taken over during the second wave of pandemic.
In continuation of its efforts, during the recently concluded Global Healthcare Summit in Hyderabad, AAPI donated immunoanalyzer at AIIMS, Bibinagar, Telangana, which does hundreds of tests every day. This is part of Covid relief efforts AAPI has taken over during the second wave of pandemic. AAPI coordinated with dozens of physicians including primary care physicians, ER, critical care and ID physicians, who see these patients on a constant basis, to help during this crisis. Questions are being sent by email and physicians answer them at the earliest convenience.
AAPI coordinated with dozens of physicians including primary care physicians, ER, critical care and ID physicians, who see these patients on a constant basis, to help during this crisis. Questions are being sent by email and physicians answer them at the earliest convenience. Dr. Anupama Gotimukula, president of AAPI along with Dr. Satheesh Kathula, AAPI secretary, and Dr. Sujeeth Punnam, Chair, Chair, Covid relief committee participated in the inauguration of biochemistry lab/Immunoanalyzer at AIIMS, Bibinagar, Hyderabad. Later on they planted trees in AIIMS Vatika, Bibinagar and named one of them “AAPI”. For more details, please visit:
Dr. Anupama Gotimukula, president of AAPI along with Dr. Satheesh Kathula, AAPI secretary, and Dr. Sujeeth Punnam, Chair, Chair, Covid relief committee participated in the inauguration of biochemistry lab/Immunoanalyzer at AIIMS, Bibinagar, Hyderabad. Later on they planted trees in AIIMS Vatika, Bibinagar and named one of them “AAPI”. For more details, please visit: 
 “During the 15th annual Global Healthcare Summit, organized in Hyderabad, India from January 5th to 7th, 2022, physician leaders from the United States and India had an opportunity to brainstorm and explore ways to focus on the theme, “Transformation of Healthcare through Telehealth and Technology usage during this post-Covid Era,” and have recommended possible ways to plan and implement preventive medicine that will save resources and precious human lives,” said Dr. Anupama Gotimukula, President of AAPI.
“During the 15th annual Global Healthcare Summit, organized in Hyderabad, India from January 5th to 7th, 2022, physician leaders from the United States and India had an opportunity to brainstorm and explore ways to focus on the theme, “Transformation of Healthcare through Telehealth and Technology usage during this post-Covid Era,” and have recommended possible ways to plan and implement preventive medicine that will save resources and precious human lives,” said Dr. Anupama Gotimukula, President of AAPI. “With numerous initiatives, AAPI has come a long way since its inception and has proved to be beneficial not only to Indian-origin American Physicians, but to Indian healthcare as well,” Mr. Naidu observed. He urged the medical fraternity and told them, “as you seek excellence in human health and well-being, do not forget the power of a kind human touch when treating your patients.”
“With numerous initiatives, AAPI has come a long way since its inception and has proved to be beneficial not only to Indian-origin American Physicians, but to Indian healthcare as well,” Mr. Naidu observed. He urged the medical fraternity and told them, “as you seek excellence in human health and well-being, do not forget the power of a kind human touch when treating your patients.” The groundbreaking Global Healthcare Summit (GHS) organized by AAPI in collaboration with the Government of India, BAPIO & GAPIO, as well as Host Alumni Chapters, including OGKTMA, ATMGUSA, KAMCOSA, and GMCGA, was packed with programs that were treat to the hearts and souls of every participant.
The groundbreaking Global Healthcare Summit (GHS) organized by AAPI in collaboration with the Government of India, BAPIO & GAPIO, as well as Host Alumni Chapters, including OGKTMA, ATMGUSA, KAMCOSA, and GMCGA, was packed with programs that were treat to the hearts and souls of every participant. Dr. Ravi Kolli, President-Elect f AAPI said, “We have made great strides in helping people to live longer, however, people are spending too many years in poor health, and these gains in health not felt equally across society. We need to focus on the rising levels of obesity, mental illness, addictions, age-related conditions like dementia, and a growing, ageing, and diverse populations, We also need to be aware of cyberbullying, pervasive misinformation and other harmful social media influences affecting our youth.”
Dr. Ravi Kolli, President-Elect f AAPI said, “We have made great strides in helping people to live longer, however, people are spending too many years in poor health, and these gains in health not felt equally across society. We need to focus on the rising levels of obesity, mental illness, addictions, age-related conditions like dementia, and a growing, ageing, and diverse populations, We also need to be aware of cyberbullying, pervasive misinformation and other harmful social media influences affecting our youth.” Dr. Krishan Kumar, Treasurer of AAPI, pointed out, “India, thus needs to redouble and continue its efforts and dedicate resources to tackle these perennial challenges. Many of these projects and programs need regular funding, and management of resources. We are grateful to dozens of AAPI members who have committed to serve India with an ongoing commitment.”
Dr. Krishan Kumar, Treasurer of AAPI, pointed out, “India, thus needs to redouble and continue its efforts and dedicate resources to tackle these perennial challenges. Many of these projects and programs need regular funding, and management of resources. We are grateful to dozens of AAPI members who have committed to serve India with an ongoing commitment.” The topics for CMEs broadly covered the recent advances in Medicine. Workshops on Medical Education and Reforms in India, Psychiatry, Palliative Care and Diabetes as well the seminar on Lifestyle Medicine led by world renowned leader and founder of Life Style Medicine, Dr. Neil Bernard were educative and offered new awareness on trends in medicine and healthier living. The Tuberclosis Awareness Seminar focused on recent advances in the TB epidemic.
The topics for CMEs broadly covered the recent advances in Medicine. Workshops on Medical Education and Reforms in India, Psychiatry, Palliative Care and Diabetes as well the seminar on Lifestyle Medicine led by world renowned leader and founder of Life Style Medicine, Dr. Neil Bernard were educative and offered new awareness on trends in medicine and healthier living. The Tuberclosis Awareness Seminar focused on recent advances in the TB epidemic. The CEO Forum, chaired by Dr. Joseph Chalil had a galaxy of CEOs from India and the United States, who shared their insights into the challenges and opportunities for making healthcare affordable, using modern technology and scientific research, Sangita Reddy, Joint MD of Apollo group of hospitals and incoming Chairman of FICCI shared her passion for the care of the masses, using technology to reach out. She praised AAPI’s efforts to help India through its Healthcare Summits in making policies in healthcare delivery more effective.
The CEO Forum, chaired by Dr. Joseph Chalil had a galaxy of CEOs from India and the United States, who shared their insights into the challenges and opportunities for making healthcare affordable, using modern technology and scientific research, Sangita Reddy, Joint MD of Apollo group of hospitals and incoming Chairman of FICCI shared her passion for the care of the masses, using technology to reach out. She praised AAPI’s efforts to help India through its Healthcare Summits in making policies in healthcare delivery more effective. “January is #CervicalCancer Awareness Month! In coordination with the local organizers of the GHS, AAPI is donating funds for the HPV Vaccination, a total of 200 doses of the vaccine for 100 children from the state of Telangana on January 9th,” said Dr. Meher Medavaram, an organizer of the program. “AAPI’s this new initiative through education and awareness programs, is aimed at help save millions of lives in India,” she added.
“January is #CervicalCancer Awareness Month! In coordination with the local organizers of the GHS, AAPI is donating funds for the HPV Vaccination, a total of 200 doses of the vaccine for 100 children from the state of Telangana on January 9th,” said Dr. Meher Medavaram, an organizer of the program. “AAPI’s this new initiative through education and awareness programs, is aimed at help save millions of lives in India,” she added. The Pre-Tour of the GHS 2019 took the delegates to the serene Kanha Shanti Vanam, located in the suburbs of Hyderabad. Magnificent in its conception and design, tranquil in its atmosphere, Kanha, blending the beauty of nature with sprawling facilities gave an inspiring experience to AAPI members an opportunity to learn to relax and meditate, through the Heartfulness movement.
The Pre-Tour of the GHS 2019 took the delegates to the serene Kanha Shanti Vanam, located in the suburbs of Hyderabad. Magnificent in its conception and design, tranquil in its atmosphere, Kanha, blending the beauty of nature with sprawling facilities gave an inspiring experience to AAPI members an opportunity to learn to relax and meditate, through the Heartfulness movement. During his address to the AAPI delegates on Jan 6th, DAAJI inspired the audience with his enriching address focusing on modern day life, the stressors and the challenges, while offering insights into how stress relaxation, meditation and cleansing would help human beings lead a peaceful life.
During his address to the AAPI delegates on Jan 6th, DAAJI inspired the audience with his enriching address focusing on modern day life, the stressors and the challenges, while offering insights into how stress relaxation, meditation and cleansing would help human beings lead a peaceful life.


 “With numerous initiatives, AAPI has come a long way since its inception and has proved to be beneficial not only to Indian-origin American Physicians, but to Indian healthcare as well,” Mr. Naidu observed. He urged the medical fraternity and told them, “as you seek excellence in human health and well-being, do not forget the power of a kind human touch when treating your patients.”
“With numerous initiatives, AAPI has come a long way since its inception and has proved to be beneficial not only to Indian-origin American Physicians, but to Indian healthcare as well,” Mr. Naidu observed. He urged the medical fraternity and told them, “as you seek excellence in human health and well-being, do not forget the power of a kind human touch when treating your patients.” In her welcome address, Dr. Anupama Gotimukula, President of AAPI, said, “This year’s Summit is focused on the theme: “Prevention is better than cure” through Technology, Telemedicine, and Transformation from the current disease-care system to a preventive healthcare system.” Dr. Gotimukula, who has chosen to focus on the “Adopt a Village” Rural Preventive Healthcare screening initiative, stated that “AAPI has brought to the attention of the Government of India the need for preventive health care screening to help detect diseases at an early stage and our purpose of the Global health summit is to interact and collaborate with Government of India and emphasize the need of annual preventive healthcare screening and have the healthcare accessible and affordable.”
In her welcome address, Dr. Anupama Gotimukula, President of AAPI, said, “This year’s Summit is focused on the theme: “Prevention is better than cure” through Technology, Telemedicine, and Transformation from the current disease-care system to a preventive healthcare system.” Dr. Gotimukula, who has chosen to focus on the “Adopt a Village” Rural Preventive Healthcare screening initiative, stated that “AAPI has brought to the attention of the Government of India the need for preventive health care screening to help detect diseases at an early stage and our purpose of the Global health summit is to interact and collaborate with Government of India and emphasize the need of annual preventive healthcare screening and have the healthcare accessible and affordable.” “We thank all the AAPI Members who are sparing their valuable time to come over to Hyderabad in order to attend this event, despite the ongoing situation of the existence of Omicron and travel restrictions. We really appreciate this gesture of courage and confidence displayed by you on behalf of Local Org. Committee, for braving odds and attending the 15th Annual AAPI GHS, Hyderabad. This is highly admirable,” said Dr. D. Dwarakanatha Reddy, India Chair, AAPI GHS 2022.
“We thank all the AAPI Members who are sparing their valuable time to come over to Hyderabad in order to attend this event, despite the ongoing situation of the existence of Omicron and travel restrictions. We really appreciate this gesture of courage and confidence displayed by you on behalf of Local Org. Committee, for braving odds and attending the 15th Annual AAPI GHS, Hyderabad. This is highly admirable,” said Dr. D. Dwarakanatha Reddy, India Chair, AAPI GHS 2022. Dr. Krishan Kumar, Treasurer of AAPI, pointed out, “India, thus needs to redouble and continue its efforts and dedicate resources to tackle these perennial challenges. Many of these projects and programs need regular funding, and management of resources. We are grateful to dozens of AAPI members who have committed to serve India with an ongoing commitment.”
Dr. Krishan Kumar, Treasurer of AAPI, pointed out, “India, thus needs to redouble and continue its efforts and dedicate resources to tackle these perennial challenges. Many of these projects and programs need regular funding, and management of resources. We are grateful to dozens of AAPI members who have committed to serve India with an ongoing commitment.” Calling it an important initiative, he praised AAPI for its “awareness program for CPR (Cardiopulmonary Resuscitation). At a time of increasing share of Non-Communicable Diseases, especially those related to the heart, we need greater awareness among people to apply CPR as a lifesaving first-aid technique and save lives during heart attacks or near drowning. I believe school children, at least at higher secondary level, and in fact, every citizen, must be taught CPR along with other basic aspects of first-aid,” her added.
Calling it an important initiative, he praised AAPI for its “awareness program for CPR (Cardiopulmonary Resuscitation). At a time of increasing share of Non-Communicable Diseases, especially those related to the heart, we need greater awareness among people to apply CPR as a lifesaving first-aid technique and save lives during heart attacks or near drowning. I believe school children, at least at higher secondary level, and in fact, every citizen, must be taught CPR along with other basic aspects of first-aid,” her added. These Indian-origin physicians are a personification of our nation’s cherished civilisational value of ‘Vasudhaiva Kutumbakam’. They are among the most successful ambassadors of India’s value systems and propagators of our mission to ‘Share and Care’ for all the people of the world, irrespective of their nationalities. We are indeed proud of them and their services.
These Indian-origin physicians are a personification of our nation’s cherished civilisational value of ‘Vasudhaiva Kutumbakam’. They are among the most successful ambassadors of India’s value systems and propagators of our mission to ‘Share and Care’ for all the people of the world, irrespective of their nationalities. We are indeed proud of them and their services. To bridge the gap between urban and rural communities, the Vice President suggested seriously exploring the use of telehealth and other technological solutions in reaching out better to rural and remote areas. “This will expand the utilization of our limited manpower and health infrastructure to reach the last mile,” he said.
To bridge the gap between urban and rural communities, the Vice President suggested seriously exploring the use of telehealth and other technological solutions in reaching out better to rural and remote areas. “This will expand the utilization of our limited manpower and health infrastructure to reach the last mile,” he said.
 The United States Senate Majority Leader Chuck Schumer, chief guest at the event, in his address, praised the contributions of Indian Americans to the larger American society. He lauded the great contributions of the largest AAPI Chapter with over 850 Member Physicians, who serve the state of New York in various capacities. “For 25 years, members of AAPI QLI has worked tirelessly to support Indian American physicians excel in patient care , teaching and research,” he said.
The United States Senate Majority Leader Chuck Schumer, chief guest at the event, in his address, praised the contributions of Indian Americans to the larger American society. He lauded the great contributions of the largest AAPI Chapter with over 850 Member Physicians, who serve the state of New York in various capacities. “For 25 years, members of AAPI QLI has worked tirelessly to support Indian American physicians excel in patient care , teaching and research,” he said. “I am grateful anmd stand here with adeep sense of gratitude and appreciation. You all esteemed members of AAPI QLI have given me tremendous opportunity to be your president during the very special year a silver jubilee year of AAPIQLI and to serve as the Chair of the Jubilee Celebrations. It has been my pleasure and very special privilege to serve as your president during silver jubilee year of AAPIQLI.”
“I am grateful anmd stand here with adeep sense of gratitude and appreciation. You all esteemed members of AAPI QLI have given me tremendous opportunity to be your president during the very special year a silver jubilee year of AAPIQLI and to serve as the Chair of the Jubilee Celebrations. It has been my pleasure and very special privilege to serve as your president during silver jubilee year of AAPIQLI.”
 The Indian American community-focused program was jointly developed by Dr. Vemuri S Murthy, Chairman of the Board of Chicago Medical Society and Founder of the Chicago Medical Society Community Bystander CPR project “SMILE” (Saving More Illinois Lives through Education) in association with Dr. Srinivas Ramaka, an eminent Cardiologist from Telangana, India. The program was attended by several members of the Indian diaspora, leaders of Medical Organizations, and Diplomats of the Indian Consulate, staff, and families.
The Indian American community-focused program was jointly developed by Dr. Vemuri S Murthy, Chairman of the Board of Chicago Medical Society and Founder of the Chicago Medical Society Community Bystander CPR project “SMILE” (Saving More Illinois Lives through Education) in association with Dr. Srinivas Ramaka, an eminent Cardiologist from Telangana, India. The program was attended by several members of the Indian diaspora, leaders of Medical Organizations, and Diplomats of the Indian Consulate, staff, and families. In his address, Hon’ble Member of Congress Danny K. Davis stressed the importance of taking care of one’s health. He commended the significant role of the Indian American doctors in contributing to the general health and well-being of US communities. In a virtual message, Honorable Congressman Raja Krishnamoorthi congratulated the Indian Consulate and Dr. Vemuri Murthy for organizing the program and their efforts to enhance outcomes after cardiac arrests among the communities.
In his address, Hon’ble Member of Congress Danny K. Davis stressed the importance of taking care of one’s health. He commended the significant role of the Indian American doctors in contributing to the general health and well-being of US communities. In a virtual message, Honorable Congressman Raja Krishnamoorthi congratulated the Indian Consulate and Dr. Vemuri Murthy for organizing the program and their efforts to enhance outcomes after cardiac arrests among the communities. Efforts to raise awareness of heart disease and promote “Healthy Heart” lifestyles is essential. Heart disease is the number one Global Public Health problem. South Asians are at a four-times greater risk of heart disease than their western counterparts and have a greater chance of having a heart attack before 50 years of age. Heart attacks strike South Asian Men and Women at younger ages, and as a result, both morbidity and mortality are higher among them compared to any other ethnic group. They tend to develop heart disease ten years earlier than other groups.
Efforts to raise awareness of heart disease and promote “Healthy Heart” lifestyles is essential. Heart disease is the number one Global Public Health problem. South Asians are at a four-times greater risk of heart disease than their western counterparts and have a greater chance of having a heart attack before 50 years of age. Heart attacks strike South Asian Men and Women at younger ages, and as a result, both morbidity and mortality are higher among them compared to any other ethnic group. They tend to develop heart disease ten years earlier than other groups.
 The U.S. never had a nationwide lockdown like other nations did. Even during the height of the pandemic in the spring of 2020, each governor made his or her own decisions about the level of restrictions to enact state by state.
The U.S. never had a nationwide lockdown like other nations did. Even during the height of the pandemic in the spring of 2020, each governor made his or her own decisions about the level of restrictions to enact state by state.

 That analysis included all cases of COVID-19 confirmed by PCR tests in England in the first half of December in which the variant could be identified: 56,000 cases of omicron and 269,000 cases of delta.
That analysis included all cases of COVID-19 confirmed by PCR tests in England in the first half of December in which the variant could be identified: 56,000 cases of omicron and 269,000 cases of delta.
 The Food and Drug Administration authorized Pfizer’s drug for adults and children ages 12 and older with a positive COVID-19 test and early symptoms who face the highest risks of hospitalization. That includes older people and those with conditions like obesity and heart disease, though the drug is not recommended for patients with severe kidney or liver problems. Children eligible for the drug must weigh at least 88 pounds (40 kilograms).
The Food and Drug Administration authorized Pfizer’s drug for adults and children ages 12 and older with a positive COVID-19 test and early symptoms who face the highest risks of hospitalization. That includes older people and those with conditions like obesity and heart disease, though the drug is not recommended for patients with severe kidney or liver problems. Children eligible for the drug must weigh at least 88 pounds (40 kilograms).


 Recent studies of the Pfizer/BioNTech vaccine showed it produced far fewer neutralising antibodies against Omicron than against the original strain, but that this deficit could be reversed by a third, booster, jab. Dr. Tedros said boosters could play an important role in curbing the spread of Covid-19, but that it was “a question of prioritization”.
Recent studies of the Pfizer/BioNTech vaccine showed it produced far fewer neutralising antibodies against Omicron than against the original strain, but that this deficit could be reversed by a third, booster, jab. Dr. Tedros said boosters could play an important role in curbing the spread of Covid-19, but that it was “a question of prioritization”.
 “It was a long-time dream of MOCAAPI members to make an impactful donation which is being fulfilled today by making a $150,000 donation to Fulfill Food Bank of Monmouth Ocean Counties and $150,000 to the Indian Cultural & Community Center to build a much-needed Community Hall in Toms River,” MOCAAPI President Dr. Avinash Gupta is quoted saying in the press release.
“It was a long-time dream of MOCAAPI members to make an impactful donation which is being fulfilled today by making a $150,000 donation to Fulfill Food Bank of Monmouth Ocean Counties and $150,000 to the Indian Cultural & Community Center to build a much-needed Community Hall in Toms River,” MOCAAPI President Dr. Avinash Gupta is quoted saying in the press release.
 The eye drops will work best for people between the ages of 40 and 55, a Vuity spokesperson told CBS. That age group comprised two clinical trials and is most likely to notice the onset of near vision loss.
The eye drops will work best for people between the ages of 40 and 55, a Vuity spokesperson told CBS. That age group comprised two clinical trials and is most likely to notice the onset of near vision loss. 
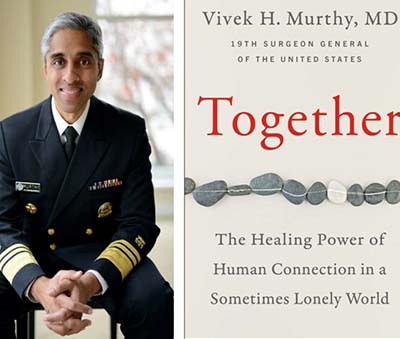 “Mental health challenges in children, adolescents, and young adults are real and widespread. Even before the pandemic, an alarming number of young people struggled with feelings of helplessness, depression, and thoughts of suicide — and rates have increased over the past decade.” Murthy is quoted saying in the press release.
“Mental health challenges in children, adolescents, and young adults are real and widespread. Even before the pandemic, an alarming number of young people struggled with feelings of helplessness, depression, and thoughts of suicide — and rates have increased over the past decade.” Murthy is quoted saying in the press release.
 In a series of over 25 comprehensive videos, Dr. Shippy shares her recommendations and action steps on what you can do now to help prepare your body so that you’ll be better equipped to resist and fight infection. This program includes everything from diet recommendations, treatment protocols and lifestyle choices to help you elevate and improve your immune system naturally while helping to support lifelong wellness.
In a series of over 25 comprehensive videos, Dr. Shippy shares her recommendations and action steps on what you can do now to help prepare your body so that you’ll be better equipped to resist and fight infection. This program includes everything from diet recommendations, treatment protocols and lifestyle choices to help you elevate and improve your immune system naturally while helping to support lifelong wellness.

 “As COVID-19 was sweeping through the nation, we at BIDMC were preparing for the projected influx of highly infectious, critically ill patients,” said lead author Sharon C. O’Donoghue, DNP, RN, a nurse specialist in the medical intensive care units at BIDMC. “It rapidly became apparent that a plan for the arrival of highly infectious critically ill patients as well as a strategy for adequate staffing protecting employees and assuring the public that this could be managed successfully were needed.”
“As COVID-19 was sweeping through the nation, we at BIDMC were preparing for the projected influx of highly infectious, critically ill patients,” said lead author Sharon C. O’Donoghue, DNP, RN, a nurse specialist in the medical intensive care units at BIDMC. “It rapidly became apparent that a plan for the arrival of highly infectious critically ill patients as well as a strategy for adequate staffing protecting employees and assuring the public that this could be managed successfully were needed.”
 According to The American Cancer Society, Cervical Cancer was once one of the most common causes of cancer death for American women. The cervical cancer death rate dropped significantly with the increased use of the Pap test for screening. Cervical cancer is among a number of cancers that can be caused by infections with pathogens – bacteria, viruses, and parasites.
According to The American Cancer Society, Cervical Cancer was once one of the most common causes of cancer death for American women. The cervical cancer death rate dropped significantly with the increased use of the Pap test for screening. Cervical cancer is among a number of cancers that can be caused by infections with pathogens – bacteria, viruses, and parasites. Dr. Anjana Samadder, Vice President of AAPI, said, “In addition to Cervical cancer, GHS 2022 will also focus on: Chronic diseases which can be prevented- notably diabetes, cardiovascular, hypertension, COPD, oncology, maternal and infant mortality, Mmanagement of neurological emergencies ENLS a certification course are only some of those that are going to be covered during this Summit.”
Dr. Anjana Samadder, Vice President of AAPI, said, “In addition to Cervical cancer, GHS 2022 will also focus on: Chronic diseases which can be prevented- notably diabetes, cardiovascular, hypertension, COPD, oncology, maternal and infant mortality, Mmanagement of neurological emergencies ENLS a certification course are only some of those that are going to be covered during this Summit.”
 ”This drive was a team effort on the part of Dr. Kishori Veerabhadrappa, Dr. Sanket Dalwadi, Dr. Jumee Barooha and Red Cross representative Heidi Deleo,” Dr. Pancholi added. Excited about the very positive and encouraging support from the community, Dr. Pancholi said, “We plan to conduct future blood drives in the 11 counties that north eastern Pennsylvania.
”This drive was a team effort on the part of Dr. Kishori Veerabhadrappa, Dr. Sanket Dalwadi, Dr. Jumee Barooha and Red Cross representative Heidi Deleo,” Dr. Pancholi added. Excited about the very positive and encouraging support from the community, Dr. Pancholi said, “We plan to conduct future blood drives in the 11 counties that north eastern Pennsylvania. “On the occasion of the 75thIndependence Day of India, we the physicians of Indian origin serving every 7th patient in the United States, are excited to launch this unique and noble initiative and Stem Cell Drive” in 75 cities across the United States,” Dr. Gotimukula added.
“On the occasion of the 75thIndependence Day of India, we the physicians of Indian origin serving every 7th patient in the United States, are excited to launch this unique and noble initiative and Stem Cell Drive” in 75 cities across the United States,” Dr. Gotimukula added.
 “Thank you all for your generous support and help in making the Blood Drive very successful,” said Dr. Jaya Daptardar. ”This drive was a team effort. I want to express my gratitude to Dr. Sushil Gupta, President of CAAPI, Dr. Subbarao Bollepalli, Viji Kurup and family members of CAPI, who came in attendance and to donate blood and support this noble initiative.” “I am grateful to First Selectwoman of Weston Samantha Nestor and Toni Boucher for gracing the event with their presence and for their support,” said Dr. Ram Chirunomula.
“Thank you all for your generous support and help in making the Blood Drive very successful,” said Dr. Jaya Daptardar. ”This drive was a team effort. I want to express my gratitude to Dr. Sushil Gupta, President of CAAPI, Dr. Subbarao Bollepalli, Viji Kurup and family members of CAPI, who came in attendance and to donate blood and support this noble initiative.” “I am grateful to First Selectwoman of Weston Samantha Nestor and Toni Boucher for gracing the event with their presence and for their support,” said Dr. Ram Chirunomula. “On the occasion of the 75thIndependence Day of India, we the physicians of Indian origin serving every 7th patient in the United States, are excited to launch this unique and noble initiative in 75 cities across the United States,” Dr. Gotimukula added.
“On the occasion of the 75thIndependence Day of India, we the physicians of Indian origin serving every 7th patient in the United States, are excited to launch this unique and noble initiative in 75 cities across the United States,” Dr. Gotimukula added.
 FIA’s General Secretary Richa Chand conducted the proceedings of the Annual Board Meeting for the year 2021-2022 and invited Founder President Sunil Shah for his opening remarks. Shahin his speech, outlined the successes behind the year 2021, listing the events conducted by the FIA and its team. He thanked the outgoing team for its hard work in putting together and conducting various India-centric and Charitable events during the year. He also took the opportunity to welcome new members to team FIA. In a major announcement, he declared that FIA would initiate an annual FIA Scholarship for deserving students starting from the year 2022.
FIA’s General Secretary Richa Chand conducted the proceedings of the Annual Board Meeting for the year 2021-2022 and invited Founder President Sunil Shah for his opening remarks. Shahin his speech, outlined the successes behind the year 2021, listing the events conducted by the FIA and its team. He thanked the outgoing team for its hard work in putting together and conducting various India-centric and Charitable events during the year. He also took the opportunity to welcome new members to team FIA. In a major announcement, he declared that FIA would initiate an annual FIA Scholarship for deserving students starting from the year 2022.
 “Though it’s too early to make any definitive statements about it, thus far it does not look like there’s a great degree of severity to it,” Fauci was quoted as saying on CNN’s ‘State of the Union on Sunday.
“Though it’s too early to make any definitive statements about it, thus far it does not look like there’s a great degree of severity to it,” Fauci was quoted as saying on CNN’s ‘State of the Union on Sunday.
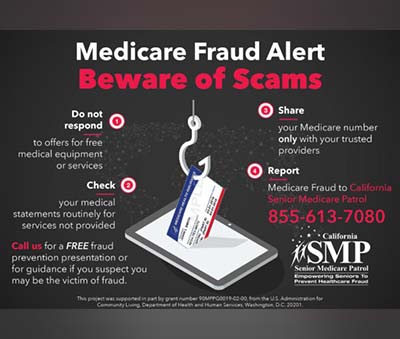 Some common examples of Medicare fraud include billing for services that were not provided, over billing, billing unnecessary services, misrepresenting dates of service or providers of service, and paying kickbacks for patient referrals.
Some common examples of Medicare fraud include billing for services that were not provided, over billing, billing unnecessary services, misrepresenting dates of service or providers of service, and paying kickbacks for patient referrals.
 Globally, more than a billion people suffer from hypertension (high blood pressure), putting them at greater risk of
Globally, more than a billion people suffer from hypertension (high blood pressure), putting them at greater risk of 
 The host chapter- AAPI-TN presented FFLI with a fundraised $75,000, in order to help strengthen the efforts to end human trafficking and to help continue and expand their impact in India.
The host chapter- AAPI-TN presented FFLI with a fundraised $75,000, in order to help strengthen the efforts to end human trafficking and to help continue and expand their impact in India. The underlying theme of Diwali, celebrating Light over Darkness, Victory of Good over Evil and Knowledge over Ignorance, which has caught up the attention of people all over the world, was done as the traditional lamp was lit by AAPI-TN Executive Committee, AAPI USA President Dr. Anupama Gotimukula, Congressman Jim Cooper and Grand Sponsor Dr. Bharat Sangani.
The underlying theme of Diwali, celebrating Light over Darkness, Victory of Good over Evil and Knowledge over Ignorance, which has caught up the attention of people all over the world, was done as the traditional lamp was lit by AAPI-TN Executive Committee, AAPI USA President Dr. Anupama Gotimukula, Congressman Jim Cooper and Grand Sponsor Dr. Bharat Sangani. Evolving to meet the growing needs of its members and the larger population it is called to serve, AAPI, the largest ethnic physician organization in the United states, representing over 100,000 Indian American Physicians, has grown steadily and is recognized by the authorities, local communities and mainstream media for the many noble initiatives AAPI has led, especially during the Covid pandemic, she said.
Evolving to meet the growing needs of its members and the larger population it is called to serve, AAPI, the largest ethnic physician organization in the United states, representing over 100,000 Indian American Physicians, has grown steadily and is recognized by the authorities, local communities and mainstream media for the many noble initiatives AAPI has led, especially during the Covid pandemic, she said. During the CMEs, several important topics with recent advances were well received by the AAPI fraternity. Themes for the CMEs included: ‘Cancer therapy: Advancement as we head for a cure’ by Dr. Nishitha Reddy, ‘Psychiatric sequelae of human trafficking’ by Dr. Sricharan Moturi, ‘Cardiovascular disease in South Asians- (Masala Study)’ by Dr. Ramya Suryadevara and ‘Stem cell therapy: The future of medicine’ by Dr. Sai Ram Atluri. The CME was well-attended, with active engagement between speakers and moderators (Dr. Amit Keswani, Dr.Varun Dhulipala, Dr. Biliyar, and Dr. Gunuganti. Attendees were eligible for 3 Category 1 CME hours, accredited by the Chicago Medical Society (CMS).
During the CMEs, several important topics with recent advances were well received by the AAPI fraternity. Themes for the CMEs included: ‘Cancer therapy: Advancement as we head for a cure’ by Dr. Nishitha Reddy, ‘Psychiatric sequelae of human trafficking’ by Dr. Sricharan Moturi, ‘Cardiovascular disease in South Asians- (Masala Study)’ by Dr. Ramya Suryadevara and ‘Stem cell therapy: The future of medicine’ by Dr. Sai Ram Atluri. The CME was well-attended, with active engagement between speakers and moderators (Dr. Amit Keswani, Dr.Varun Dhulipala, Dr. Biliyar, and Dr. Gunuganti. Attendees were eligible for 3 Category 1 CME hours, accredited by the Chicago Medical Society (CMS). The gala began with the Event Chair Dr. Sunil Kaza welcoming community members, family, friends, colleagues and sponsors. “We, AAPI- TN team, worked hard to stick to the mission of AAPI, for education and charity to serve humanity. We thank each and every member that attended and supported the event. Our special thanks to all our Sponsors,” said Dr. Sunil Kaza, Chair of the Gala Committee. The Grand sponsor for the event, Dr. Bharat Sangani attended the meeting personally.
The gala began with the Event Chair Dr. Sunil Kaza welcoming community members, family, friends, colleagues and sponsors. “We, AAPI- TN team, worked hard to stick to the mission of AAPI, for education and charity to serve humanity. We thank each and every member that attended and supported the event. Our special thanks to all our Sponsors,” said Dr. Sunil Kaza, Chair of the Gala Committee. The Grand sponsor for the event, Dr. Bharat Sangani attended the meeting personally.
 Physicians and other health professionals on the front lines of COVID-19 care have experienced so many unknowns during the pandemic. They’ve also put their own health and the well-being of their families on the line to provide care.
Physicians and other health professionals on the front lines of COVID-19 care have experienced so many unknowns during the pandemic. They’ve also put their own health and the well-being of their families on the line to provide care. AAPI’s participation at the Marathon was inspired and sponsored by the Botla Foundation, which provided a great kick start to AAPI’s wellness theme, pointed to the Six Pillars of Lifestyle Medicine: 1. Healthy Diet; 2. Being active; 3. Restorative sleep; 4. Managing stress; 5. Have social and supportive connections; and, 6. Avoiding abusive drugs and habits.
AAPI’s participation at the Marathon was inspired and sponsored by the Botla Foundation, which provided a great kick start to AAPI’s wellness theme, pointed to the Six Pillars of Lifestyle Medicine: 1. Healthy Diet; 2. Being active; 3. Restorative sleep; 4. Managing stress; 5. Have social and supportive connections; and, 6. Avoiding abusive drugs and habits. Dozens of Doctors and community leaders joined the Rock and Roll Marathon, which had attracted over 18,000 participants from around the nation, and made this an inspiring experience for all. Dr. Ravi Botla, while thanking and congratulating all the participants at the Marathon, said, “Running with you all is an amazing experience. Several friends made their personal bests today. Hope to continue to do some physical activity (running/walking/cycling) to improve our health. On behalf of all our runners yesterday and today, Botla Foundation will donate $25,000 to AAPI, irrespective of the number of participants. We should be proud of this accomplishment. Thank you Anupama and Jayesh to provide this opportunity.”
Dozens of Doctors and community leaders joined the Rock and Roll Marathon, which had attracted over 18,000 participants from around the nation, and made this an inspiring experience for all. Dr. Ravi Botla, while thanking and congratulating all the participants at the Marathon, said, “Running with you all is an amazing experience. Several friends made their personal bests today. Hope to continue to do some physical activity (running/walking/cycling) to improve our health. On behalf of all our runners yesterday and today, Botla Foundation will donate $25,000 to AAPI, irrespective of the number of participants. We should be proud of this accomplishment. Thank you Anupama and Jayesh to provide this opportunity.” “After a hiatus of 5 years from long distance running, I am thrilled to announce that I completed running the half marathon in San Antonio on a PLANT BASED DIET!” Dr. Akil Taher said. “I ran to support the American Association of Physicians of Indian origin (AAPI) under the leadership of Dr. Anupama Gotimukula ad Dr. Jayesh Shah. AAPI has done some phenomenal charity work here in the US and India. Also a big thank you to the Botla family for their inspirational support to AAPI,” he added.
“After a hiatus of 5 years from long distance running, I am thrilled to announce that I completed running the half marathon in San Antonio on a PLANT BASED DIET!” Dr. Akil Taher said. “I ran to support the American Association of Physicians of Indian origin (AAPI) under the leadership of Dr. Anupama Gotimukula ad Dr. Jayesh Shah. AAPI has done some phenomenal charity work here in the US and India. Also a big thank you to the Botla family for their inspirational support to AAPI,” he added. To run my first half-marathon with my Idol, Dr. Taher. He is a living proof of the power of ‘Whole Foods Plant Based’ Diet and Physical Exercise in not just recovering from a major surgery but healing from within for a better and stronger health than before. His presenceat the Marathon inspired us to sign up for the event and support AAPI in promoting ‘health & fitness’ in our community,” stated Dr. Bhoja R. Katipally.
To run my first half-marathon with my Idol, Dr. Taher. He is a living proof of the power of ‘Whole Foods Plant Based’ Diet and Physical Exercise in not just recovering from a major surgery but healing from within for a better and stronger health than before. His presenceat the Marathon inspired us to sign up for the event and support AAPI in promoting ‘health & fitness’ in our community,” stated Dr. Bhoja R. Katipally. The donor, Dr. Ravi Botla did his first full Marathon. There are several in the group who did their first half marathon including Dr. Jayesh Shah! We thank the Botla Foundation who inspired us! We ran with a good heart to support AAPI. Nothing is impossible if we have the motivation inside us!!” For more details on AAPI and the 40th convention, please visit:
The donor, Dr. Ravi Botla did his first full Marathon. There are several in the group who did their first half marathon including Dr. Jayesh Shah! We thank the Botla Foundation who inspired us! We ran with a good heart to support AAPI. Nothing is impossible if we have the motivation inside us!!” For more details on AAPI and the 40th convention, please visit: 
 The variant could lead to severe consequences in some regions, the WHO said on Monday. The head of the organisation, Dr Tedros Adhanom Ghebreyesus, renewed a call for a global push to get vaccines to poorer nations.
The variant could lead to severe consequences in some regions, the WHO said on Monday. The head of the organisation, Dr Tedros Adhanom Ghebreyesus, renewed a call for a global push to get vaccines to poorer nations.
 According to her, “Senior leaders from leading healthcare organizations such as pharmaceuticals, device and medical equipment manufacturers and major medical teaching institutions, hospitals and from the Ministries – Health, External/Overseas Affairs and regulatory bodies are collaborating with AAPI with the ultimate goal to provide access to high quality and affordable healthcare to all people of India.”
According to her, “Senior leaders from leading healthcare organizations such as pharmaceuticals, device and medical equipment manufacturers and major medical teaching institutions, hospitals and from the Ministries – Health, External/Overseas Affairs and regulatory bodies are collaborating with AAPI with the ultimate goal to provide access to high quality and affordable healthcare to all people of India.” Dr. Joseph Chalil, Chair of the CEO Forum said, “AAPI has made significant contributions towards addressing several issues affecting the healthcare system in India. During the GHS 2022, AAPI at the popular CEO Forum, physician leaders from the United States and India will have an opportunity to brainstorm and explore ways to focus on the theme, “Prevention is Better Than Cure” and recommend possible ways to plan and implement preventive medicine that will save resources and precious human lives.”
Dr. Joseph Chalil, Chair of the CEO Forum said, “AAPI has made significant contributions towards addressing several issues affecting the healthcare system in India. During the GHS 2022, AAPI at the popular CEO Forum, physician leaders from the United States and India will have an opportunity to brainstorm and explore ways to focus on the theme, “Prevention is Better Than Cure” and recommend possible ways to plan and implement preventive medicine that will save resources and precious human lives.”
 Burton said that researchers will know just how effective the vaccines are against this variant “in the next couple of weeks.” If manufacturers need to make an omicron variant-specific vaccine, it should take approximately “two to three months” to test and manufacture it, he said.
Burton said that researchers will know just how effective the vaccines are against this variant “in the next couple of weeks.” If manufacturers need to make an omicron variant-specific vaccine, it should take approximately “two to three months” to test and manufacture it, he said.
 “Their symptoms were so different and so mild from those I had treated before,” said Dr Coetzee, a GP for 33 years who chairs the South African Medical Association alongside running her practice.
“Their symptoms were so different and so mild from those I had treated before,” said Dr Coetzee, a GP for 33 years who chairs the South African Medical Association alongside running her practice.
 Late last week, the US announced a ban on flights from South Africa, Botswana, Zimbabwe, Namibia, Lesotho, Eswatini, Mozambique and Malawi. Canada, the UK and the EU and other countries have also restricted travel from southern Africa.
Late last week, the US announced a ban on flights from South Africa, Botswana, Zimbabwe, Namibia, Lesotho, Eswatini, Mozambique and Malawi. Canada, the UK and the EU and other countries have also restricted travel from southern Africa.
 “From the beginning, we have said that as we seek to defeat the pandemic, it is imperative that we are proactive as the virus evolves,” said Moderna CEO Stéphane Bancel. “The mutations in the Omicron variant are concerning and for several days, we have been moving as fast as possible to execute our strategy to address this variant.”
“From the beginning, we have said that as we seek to defeat the pandemic, it is imperative that we are proactive as the virus evolves,” said Moderna CEO Stéphane Bancel. “The mutations in the Omicron variant are concerning and for several days, we have been moving as fast as possible to execute our strategy to address this variant.”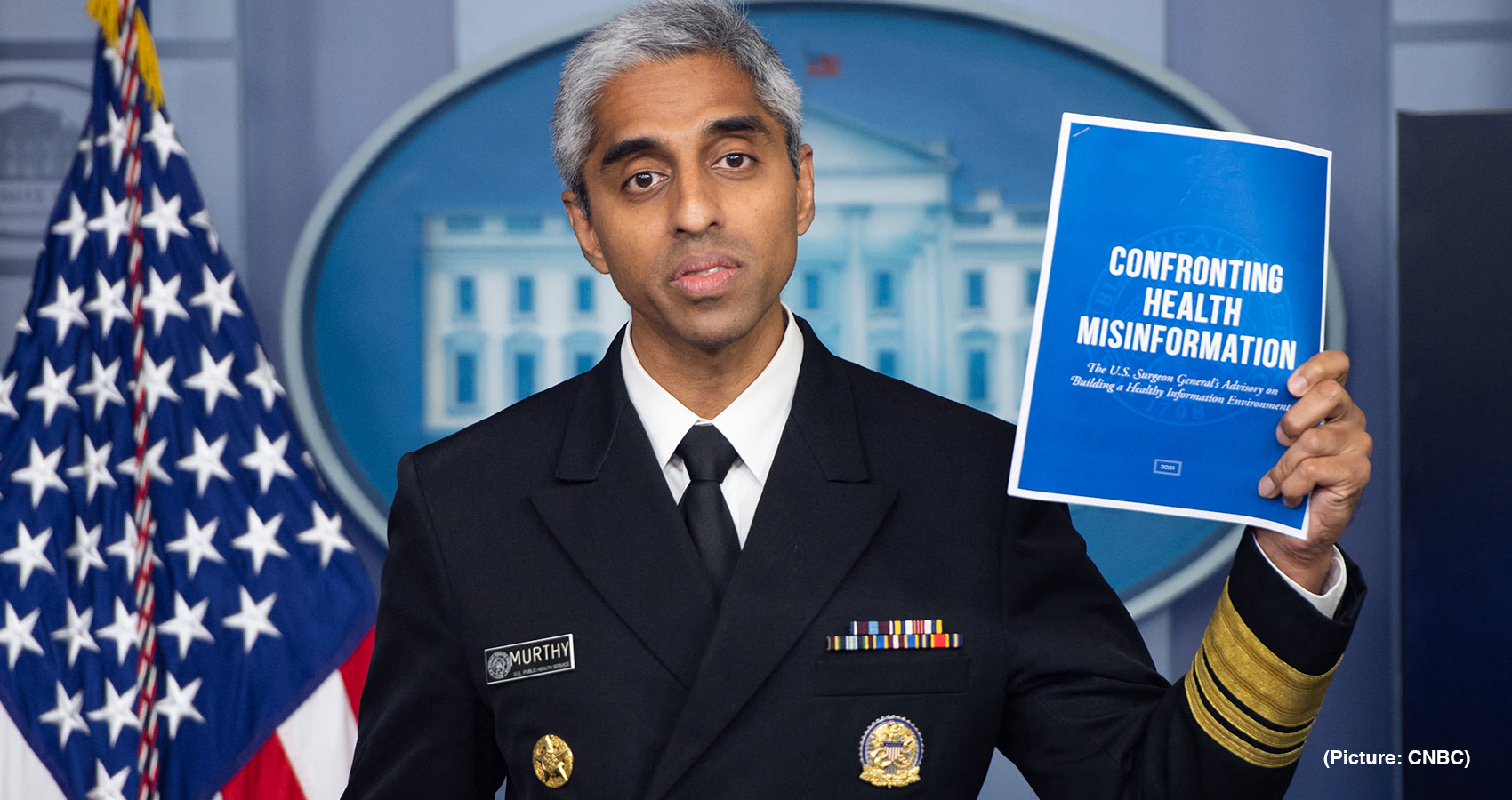
 But “I also worry about what’s happened to our clinicians. Yes, they have been absolute heroes, but that’s coming at a cost,” said Dr. Murthy. “The question that we have to ask ourselves as a country is: Are we willing to finally step up and do something?
But “I also worry about what’s happened to our clinicians. Yes, they have been absolute heroes, but that’s coming at a cost,” said Dr. Murthy. “The question that we have to ask ourselves as a country is: Are we willing to finally step up and do something?
 The Ministry also issued an advisory to all ASU Drugs Manufacturers Associations seeking the manufacturers of the crude drug/extracts, sellers, ASU drug manufacturing companies, ASU drug exporters not to use Withania somnifera leaves either in crude or extract or any other form for therapeutic purposes under the ambit of ASU drugs.
The Ministry also issued an advisory to all ASU Drugs Manufacturers Associations seeking the manufacturers of the crude drug/extracts, sellers, ASU drug manufacturing companies, ASU drug exporters not to use Withania somnifera leaves either in crude or extract or any other form for therapeutic purposes under the ambit of ASU drugs.
 The World Health Organization says that cancer is diagnosed in more than 14 million people worldwide annually and ends up killing approximately 8.8 million. What is most shocking is that two-thirds of these deaths are in low-middle income countries where diagnosis is found to be inadequate.
The World Health Organization says that cancer is diagnosed in more than 14 million people worldwide annually and ends up killing approximately 8.8 million. What is most shocking is that two-thirds of these deaths are in low-middle income countries where diagnosis is found to be inadequate. The annual physical exam is part of the larger discussion about primary care and whether it is necessary. In the U.S., India, and other countries around the world, medicine has become the way you manage disease, not prevent it. Primary care, on the other hand, is a way to prevent disease by talking with patients about their potential health risks and giving them practical advice on how to care for their health, while considering their unique lifestyle challenges.
The annual physical exam is part of the larger discussion about primary care and whether it is necessary. In the U.S., India, and other countries around the world, medicine has become the way you manage disease, not prevent it. Primary care, on the other hand, is a way to prevent disease by talking with patients about their potential health risks and giving them practical advice on how to care for their health, while considering their unique lifestyle challenges.
 HHS
HHS 
 Overdose deaths have more than doubled since 2015, said the report, adding that it resulted from losing access to treatment, rising mental health problems and wider availability of dangerously potent street drugs.
Overdose deaths have more than doubled since 2015, said the report, adding that it resulted from losing access to treatment, rising mental health problems and wider availability of dangerously potent street drugs.

 Happiness can only grow and flourish in a peaceful, positive, pure and powerful mind and it will die in a mental atmosphere filled with the obstacles of negativity, anger, criticism, arrogance or depression. It is as if many of us have forgotten our original positive qualities and we have been overtaken by the negative qualities that are prevalent in our world today.
Happiness can only grow and flourish in a peaceful, positive, pure and powerful mind and it will die in a mental atmosphere filled with the obstacles of negativity, anger, criticism, arrogance or depression. It is as if many of us have forgotten our original positive qualities and we have been overtaken by the negative qualities that are prevalent in our world today.

 “Vaccination is just one tool. It’s not a silver bullet,” she told DW. “Vaccines are very effective against protecting against severe disease…But vaccines are not 100% effective against infection.”
“Vaccination is just one tool. It’s not a silver bullet,” she told DW. “Vaccines are very effective against protecting against severe disease…But vaccines are not 100% effective against infection.”
 “As the President, one of my main goal is to revitalize local Chapters that are the backbone for the national organization; help make the local Chapters financially viable as funds have dwindled due to pharma support; and to bring in younger physicians into the fold,” the young and dynamic President told a select group of audience who had come to cheer him and the new executive committee.
“As the President, one of my main goal is to revitalize local Chapters that are the backbone for the national organization; help make the local Chapters financially viable as funds have dwindled due to pharma support; and to bring in younger physicians into the fold,” the young and dynamic President told a select group of audience who had come to cheer him and the new executive committee. “I would also like to thank all the leaders of IAMA, especially Drs, Vemuri Murthy, Hanumadass, Rohit Vasa, Satya Ahuja, Shastri Swaminathan, Khandelwal, Arvind Goyal, Annita John, Utpal Parikh, Sukanya Reddy and several others.” He had a special note for Dr. Lalmalani. “I would like to thank my spiritual guru and political mentor, our Mayor of Oak Brook Dr. Lalmalani.”
“I would also like to thank all the leaders of IAMA, especially Drs, Vemuri Murthy, Hanumadass, Rohit Vasa, Satya Ahuja, Shastri Swaminathan, Khandelwal, Arvind Goyal, Annita John, Utpal Parikh, Sukanya Reddy and several others.” He had a special note for Dr. Lalmalani. “I would like to thank my spiritual guru and political mentor, our Mayor of Oak Brook Dr. Lalmalani.” Author of many international medical journal articles, Dr. Reddy has traveled extensively, giving specialty lectures on the complex procedures that he does. Active in teaching and mentoring many medical students and residents, Dr. Reddy has received numerous teaching and mentoring awards. To his credit, he is a four-time recipient of “Faculty award for excellence in teaching” awarded by the Harvard Medical Students and Residents.
Author of many international medical journal articles, Dr. Reddy has traveled extensively, giving specialty lectures on the complex procedures that he does. Active in teaching and mentoring many medical students and residents, Dr. Reddy has received numerous teaching and mentoring awards. To his credit, he is a four-time recipient of “Faculty award for excellence in teaching” awarded by the Harvard Medical Students and Residents. In the summer of 2019, Dr. Reddy organized The Global Health Summit in Hyderabad, an educational event with numerous workshops. Vice President of India, Sri Venkaiah Naidu, Union Minster of Health, Dr. Harshvardhan, both addressed the highly successful Global Health Summit. In October of 2019, he played a key role along with the Indian Resuscitation Council to train almost 500,000 lay people in Cardio-Pulmonary Resuscitation in India.
In the summer of 2019, Dr. Reddy organized The Global Health Summit in Hyderabad, an educational event with numerous workshops. Vice President of India, Sri Venkaiah Naidu, Union Minster of Health, Dr. Harshvardhan, both addressed the highly successful Global Health Summit. In October of 2019, he played a key role along with the Indian Resuscitation Council to train almost 500,000 lay people in Cardio-Pulmonary Resuscitation in India. His leadership and foresight were deeply appreciated as AAPI became the first major organization to call for universal masking. In this regard, AAPI provided free masks to thousands of health care workers. AAPI members have honored more than 10,000 nurses in over 100 hospitals across more than 40 states by sponsoring lunches for them during the Nurses Week. He was instrumental in organizing the Obesity prevention programs in all continenets, sharing medical knowledge globally, team-building activities such as the Share-A-Blanket program, medical education programs such as CPR training, morale building programs like mentoring a future medical students, and India heritage programs like Independence Day celebrations.
His leadership and foresight were deeply appreciated as AAPI became the first major organization to call for universal masking. In this regard, AAPI provided free masks to thousands of health care workers. AAPI members have honored more than 10,000 nurses in over 100 hospitals across more than 40 states by sponsoring lunches for them during the Nurses Week. He was instrumental in organizing the Obesity prevention programs in all continenets, sharing medical knowledge globally, team-building activities such as the Share-A-Blanket program, medical education programs such as CPR training, morale building programs like mentoring a future medical students, and India heritage programs like Independence Day celebrations. IAMA-IL is a non-profit organization comprised of Illinois physicians, fellows, residents, and medical students of Indian origin who are committed to professional excellence and quality patient care. IAMA-IL offers many opportunities for your organization to begin and grow a connection with our members and the communities we serve. We like to partner with organizations and people that strive for similar goals including a commitment to excellence, education, research and serving the community.
IAMA-IL is a non-profit organization comprised of Illinois physicians, fellows, residents, and medical students of Indian origin who are committed to professional excellence and quality patient care. IAMA-IL offers many opportunities for your organization to begin and grow a connection with our members and the communities we serve. We like to partner with organizations and people that strive for similar goals including a commitment to excellence, education, research and serving the community.
 In this regard, he highlighted some data points from the WHO Global Report on Traditional and Complementary Medicine 2019 – number of countries with national policy on traditional and complementary medicine has increased from 25 in 1998 to 98 in 2019 and countries with health insurance cover for traditional and complementary medicine has increased from 37 in 2012 to 45 in 2018. Consul General underlined the vast network of scientific studies being undertaken on Ayurveda in universities in the United States and in research ecosystems across the world including in India.
In this regard, he highlighted some data points from the WHO Global Report on Traditional and Complementary Medicine 2019 – number of countries with national policy on traditional and complementary medicine has increased from 25 in 1998 to 98 in 2019 and countries with health insurance cover for traditional and complementary medicine has increased from 37 in 2012 to 45 in 2018. Consul General underlined the vast network of scientific studies being undertaken on Ayurveda in universities in the United States and in research ecosystems across the world including in India.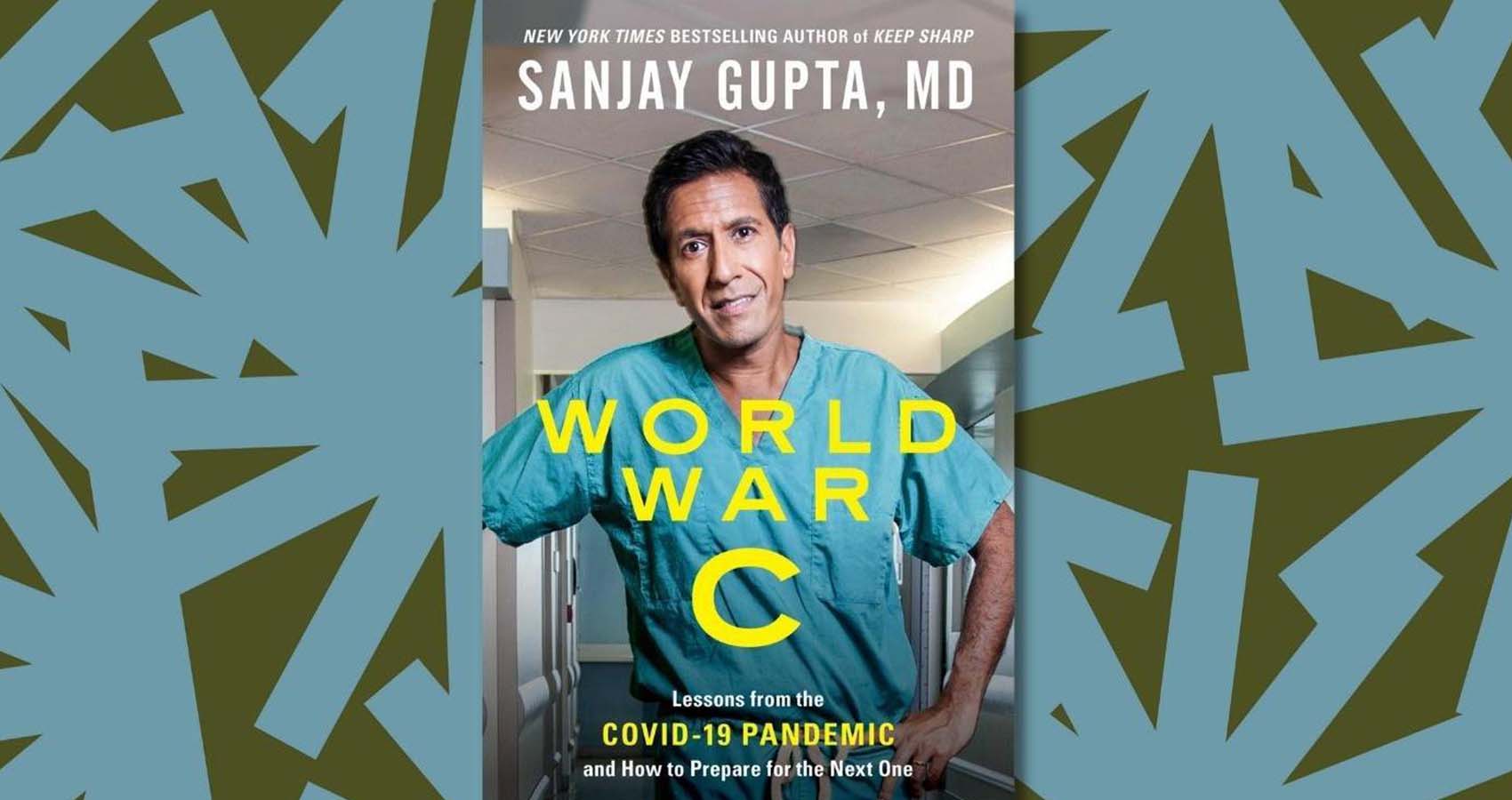
 CNN chief medical correspondent Sanjay Gupta, MD, offers an accessible, data-packed answer to our biggest questions about Covid-19: What have we learned about this pandemic and how can we prepare for—or prevent—the next one?
CNN chief medical correspondent Sanjay Gupta, MD, offers an accessible, data-packed answer to our biggest questions about Covid-19: What have we learned about this pandemic and how can we prepare for—or prevent—the next one? Gupta argues that we need to prepare for a new era where pandemics will be more frequent, and possibly even more deadly. As the doctor who’s been holding America’s hand through the crisis with compassion, clarity, and well-earned wisdom, he gives you the unvarnished story behind the pandemic, including insights about the novel virus’s behavior, and offers practical tools to ready ourselves for what lies ahead. He answers critical questions: Can we stamp out the virus for good (and if not, how do we live with it)? Should we put our parents in a nursing home? Where should we live? What should we stockpile? What should we know before taking a trip? Does it make sense to spend more on health insurance to deal with any long-term effects? How do you decide when it’s safe to go to a public pool or schedule elective surgery? What should Covid survivors know about protecting their future health? What if you become a long-hauler with chronic health challenges stemming?
Gupta argues that we need to prepare for a new era where pandemics will be more frequent, and possibly even more deadly. As the doctor who’s been holding America’s hand through the crisis with compassion, clarity, and well-earned wisdom, he gives you the unvarnished story behind the pandemic, including insights about the novel virus’s behavior, and offers practical tools to ready ourselves for what lies ahead. He answers critical questions: Can we stamp out the virus for good (and if not, how do we live with it)? Should we put our parents in a nursing home? Where should we live? What should we stockpile? What should we know before taking a trip? Does it make sense to spend more on health insurance to deal with any long-term effects? How do you decide when it’s safe to go to a public pool or schedule elective surgery? What should Covid survivors know about protecting their future health? What if you become a long-hauler with chronic health challenges stemming?
 “We invite you to the AAPI 40th Annual Convention in the beautiful city of San Antonio, Texas,” Dr. Jayesh Shah, past President of AAPI and Chair of AAPI Convention 2022 said. Welcoming the delegates to his “Home city of San Antonio,” which is hosting the 2nd national convention, Dr. Shah said, “We have convened a fantastic group of people to meet the needs of the 2022 convention and are very excited about this year. Please reach out to any one of the representatives from the San Antonio team with questions or comments.”
“We invite you to the AAPI 40th Annual Convention in the beautiful city of San Antonio, Texas,” Dr. Jayesh Shah, past President of AAPI and Chair of AAPI Convention 2022 said. Welcoming the delegates to his “Home city of San Antonio,” which is hosting the 2nd national convention, Dr. Shah said, “We have convened a fantastic group of people to meet the needs of the 2022 convention and are very excited about this year. Please reach out to any one of the representatives from the San Antonio team with questions or comments.” “Our physician members have worked very hard during the covid 19 pandemic as the 2022 convention is a perfect time to heal the healers with a special focus on wellness,” said Dr. Jayesh Shah. Accordingly, some of the major themes at the convention include: Yoga and Meditation practices, Welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, Ailment based yoga therapy sessions, Workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine, as well as a unique opportunity to visit first of its kind in San Antonio, Aum Ashram as part of the Wellness session.
“Our physician members have worked very hard during the covid 19 pandemic as the 2022 convention is a perfect time to heal the healers with a special focus on wellness,” said Dr. Jayesh Shah. Accordingly, some of the major themes at the convention include: Yoga and Meditation practices, Welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, Ailment based yoga therapy sessions, Workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine, as well as a unique opportunity to visit first of its kind in San Antonio, Aum Ashram as part of the Wellness session.

 Metkar’s identification as the “first named inventor” is in the document filed by Moderna to dispute the U.S. government’s National Institutes of Health assertion that its scientists should also be credited as inventors of the vaccine, which was developed in collaboration with it and with $1.53 billion provided by the administration of former President Donald Trump under the Operation Warp Speed program to quickly produce vaccines.
Metkar’s identification as the “first named inventor” is in the document filed by Moderna to dispute the U.S. government’s National Institutes of Health assertion that its scientists should also be credited as inventors of the vaccine, which was developed in collaboration with it and with $1.53 billion provided by the administration of former President Donald Trump under the Operation Warp Speed program to quickly produce vaccines.
 Like Pfizer-BioNTech’s adult vaccine, the pediatric version is meant to be given in two doses, spaced three weeks apart. Each dose, however, is smaller than that given to adults.
Like Pfizer-BioNTech’s adult vaccine, the pediatric version is meant to be given in two doses, spaced three weeks apart. Each dose, however, is smaller than that given to adults.
 Two studies show one of four flu viruses that infect humans each year hasn’t been detected anywhere in the world since April 2020.
Two studies show one of four flu viruses that infect humans each year hasn’t been detected anywhere in the world since April 2020.
 The Covid pandemic has impacted all aspects of human life as never been before. The past two years have been challenging to everyone, particularly those are assigned with the responsibility of caring for the sick, especially as hundreds of Millions were affected by the big pandemic. Over 115,000 health care workers died from Covid-19 from January 2020 to May of this year, according to a new World Health Organization estimate.
The Covid pandemic has impacted all aspects of human life as never been before. The past two years have been challenging to everyone, particularly those are assigned with the responsibility of caring for the sick, especially as hundreds of Millions were affected by the big pandemic. Over 115,000 health care workers died from Covid-19 from January 2020 to May of this year, according to a new World Health Organization estimate. Accordingly, some of the major themes at the convention include: Yoga and Meditation practices, Welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, Ailment based yoga therapy sessions, Workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine, as well as an unique opportunity to visit first of its kind in San Antonio, Aum Ashram as part of the Wellness session.
Accordingly, some of the major themes at the convention include: Yoga and Meditation practices, Welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, Ailment based yoga therapy sessions, Workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine, as well as an unique opportunity to visit first of its kind in San Antonio, Aum Ashram as part of the Wellness session.
 The FDA panel accepted
The FDA panel accepted 
 The TAG — which is an independent advisory group that recommends to WHO on whether a Covid-19 vaccine fulfils criteria for EUL or not — will meet next on November 3.
The TAG — which is an independent advisory group that recommends to WHO on whether a Covid-19 vaccine fulfils criteria for EUL or not — will meet next on November 3.
 Building on earlier work with Tiffany Ford from May 2020, “
Building on earlier work with Tiffany Ford from May 2020, “
 We recently learned that there are certain
We recently learned that there are certain 
 PM Narendra Modi tweeted: “The journey from anxiety to assurance has happened and our nation has emerged stronger, thanks to the world’s largest vaccination drive.”
PM Narendra Modi tweeted: “The journey from anxiety to assurance has happened and our nation has emerged stronger, thanks to the world’s largest vaccination drive.”
 Certain people who received Pfizer vaccinations months ago already are eligible for a booster and now the Centers for Disease Control and Prevention says specific Moderna and Johnson & Johnson recipients qualify, too. And in a bigger change, the agency is allowing the flexibility of “mixing and matching” that extra dose regardless of which type people received first.
Certain people who received Pfizer vaccinations months ago already are eligible for a booster and now the Centers for Disease Control and Prevention says specific Moderna and Johnson & Johnson recipients qualify, too. And in a bigger change, the agency is allowing the flexibility of “mixing and matching” that extra dose regardless of which type people received first.
 The hearings will take place one month before the Supreme Court is set to hear arguments in another pivotal abortion case, Dobbs v. Jackson Women’s Health, which directly challenges the abortion-rights precedent established in 1973 under Roe v. Wade. The court announced on Friday its decision to hear arguments over whether the Biden administration had the right to sue to end enforcement of the law, Sotomayor indicated that she
The hearings will take place one month before the Supreme Court is set to hear arguments in another pivotal abortion case, Dobbs v. Jackson Women’s Health, which directly challenges the abortion-rights precedent established in 1973 under Roe v. Wade. The court announced on Friday its decision to hear arguments over whether the Biden administration had the right to sue to end enforcement of the law, Sotomayor indicated that she 

 Led by Professor Shulamit Levenberg, Ph.D. student Rita Beckerman from the Stem Cell and Tissue Engineering Laboratory in the Technion’s Faculty of Biomedical Engineering presents a novel treatment approach, using an autograft of muscle cells engineered to take in sugar at increased rates. Mice treated in this manner displayed normal blood sugar levels for months after a single procedure. The group’s findings were recently published in
Led by Professor Shulamit Levenberg, Ph.D. student Rita Beckerman from the Stem Cell and Tissue Engineering Laboratory in the Technion’s Faculty of Biomedical Engineering presents a novel treatment approach, using an autograft of muscle cells engineered to take in sugar at increased rates. Mice treated in this manner displayed normal blood sugar levels for months after a single procedure. The group’s findings were recently published in 
 “Data from 119 countries suggest that on average, two in five healthcare workers globally are fully vaccinated,” Dr Tedros said. “But of course, that average masks huge differences across regions and economic groupings.” Fewer than one in 10 healthcare workers were fully vaccinated in Africa, he said, compared with eight in 10 in high-income countries. A failure to provide poorer countries with enough vaccines was highlighted earlier by Dr Bruce Aylward, a senior leader at the WHO, who said it meant the Covid crisis could “easily drag on deep into 2022”.
“Data from 119 countries suggest that on average, two in five healthcare workers globally are fully vaccinated,” Dr Tedros said. “But of course, that average masks huge differences across regions and economic groupings.” Fewer than one in 10 healthcare workers were fully vaccinated in Africa, he said, compared with eight in 10 in high-income countries. A failure to provide poorer countries with enough vaccines was highlighted earlier by Dr Bruce Aylward, a senior leader at the WHO, who said it meant the Covid crisis could “easily drag on deep into 2022”.
 Dr. V.K. Raju, who was born in Rajahmundry, AP, India, is a Clinical Professor of Ophthalmology at West Virginia University, Fellow of the Royal College of Surgeons, Fellow of the American College of Surgeons, Director of the International Ocular Surface Society, Director of the Ocular Surface Research and Education Foundation, Chairman of Goutami Eye Institute in Rajahmundry and is the President and Founder of the Eye Foundation of America, a non-profit organization dedicated to realizing a world without childhood blindness.
Dr. V.K. Raju, who was born in Rajahmundry, AP, India, is a Clinical Professor of Ophthalmology at West Virginia University, Fellow of the Royal College of Surgeons, Fellow of the American College of Surgeons, Director of the International Ocular Surface Society, Director of the Ocular Surface Research and Education Foundation, Chairman of Goutami Eye Institute in Rajahmundry and is the President and Founder of the Eye Foundation of America, a non-profit organization dedicated to realizing a world without childhood blindness. Dr. Raju expressed gratitude to all the Board members of the Foundation in UK, particularly, Ashwini Misro, Radhika Misro, and Raj Koppada for their enthusiasm and generosity in helping realize the mission of the Eye Foundation in preventing and treating childhood blindness and beyond in Uzbekistan.
Dr. Raju expressed gratitude to all the Board members of the Foundation in UK, particularly, Ashwini Misro, Radhika Misro, and Raj Koppada for their enthusiasm and generosity in helping realize the mission of the Eye Foundation in preventing and treating childhood blindness and beyond in Uzbekistan.
 In this context, as part of an ongoing awareness and education campaign about high risk heart disease in South Asians, American Association of Physicians of Indian Origin (AAPI) the largest ethnic medical organization in the United States presented two eminent speakers and experts, Dr. Enas Enas and Dr. Amit Kera, discussing ways to create awareness on Heart Disease Among South Asians during a webinar on Saturday, October 16th, 2021.
In this context, as part of an ongoing awareness and education campaign about high risk heart disease in South Asians, American Association of Physicians of Indian Origin (AAPI) the largest ethnic medical organization in the United States presented two eminent speakers and experts, Dr. Enas Enas and Dr. Amit Kera, discussing ways to create awareness on Heart Disease Among South Asians during a webinar on Saturday, October 16th, 2021. Dr. Enas referred to several research/studies around the world, showing high prevalence of CAD among Indians. “Indians have a big problem with premature heart disease,” Dr. Enas said and pointed out that 185,000 people of South Asian origin die of heart disease per year as against 15,000 Whites die of the same health issue. While referring to Mitigating Risk Factors, Dr. Enas recommended Indians to follow the American Heart Association developed Life Simple 7 with additional requirement for exercise and maintaining sugar level below 140.
Dr. Enas referred to several research/studies around the world, showing high prevalence of CAD among Indians. “Indians have a big problem with premature heart disease,” Dr. Enas said and pointed out that 185,000 people of South Asian origin die of heart disease per year as against 15,000 Whites die of the same health issue. While referring to Mitigating Risk Factors, Dr. Enas recommended Indians to follow the American Heart Association developed Life Simple 7 with additional requirement for exercise and maintaining sugar level below 140. Dr. Amit Kera, a new rising star in Preventive Cardiology, built on that argument and presented genomic data to fill the gap and also pointed out that usual risk scoring has been done on Caucasians and cannot be extrapolated to south Asians. He advocated for the need for our own data base and especially genomic data to go beyond coronary calcium score and use “ Polygenic score,” which can predict even more accurately the risk of heart disease individually what he calls “Precision Medicine,” a futuristic concept, which he is working on as Associate Director at prestigious Broad institute affiliated with MIT and Harvard. Pointing to international studies that point to prevalence of Cardiovascular diseases high among South Asians, he said, Diabetes is diagnosed four times more among the Asians in comparison with Europeans.
Dr. Amit Kera, a new rising star in Preventive Cardiology, built on that argument and presented genomic data to fill the gap and also pointed out that usual risk scoring has been done on Caucasians and cannot be extrapolated to south Asians. He advocated for the need for our own data base and especially genomic data to go beyond coronary calcium score and use “ Polygenic score,” which can predict even more accurately the risk of heart disease individually what he calls “Precision Medicine,” a futuristic concept, which he is working on as Associate Director at prestigious Broad institute affiliated with MIT and Harvard. Pointing to international studies that point to prevalence of Cardiovascular diseases high among South Asians, he said, Diabetes is diagnosed four times more among the Asians in comparison with Europeans.
 Binghamton University Professor of Political Science Olga Shvetsova
Binghamton University Professor of Political Science Olga Shvetsova
 The COVID-19 vaccine made by
The COVID-19 vaccine made by 
 The disease is the most prevalent form of cancer globally and has become a major problem in India, where breast cancer accounts for 25% to 31% of all cancers.
The disease is the most prevalent form of cancer globally and has become a major problem in India, where breast cancer accounts for 25% to 31% of all cancers.
 The CDC published data Oct. 15 that breaks down the rate of COVID-19 cases and deaths by vaccination status and vaccine type. The rates are based on data from 16 public health departments — representing about 30 percent of the U.S. population — and cover April through the end of August.
The CDC published data Oct. 15 that breaks down the rate of COVID-19 cases and deaths by vaccination status and vaccine type. The rates are based on data from 16 public health departments — representing about 30 percent of the U.S. population — and cover April through the end of August. 
 The $20 copay was well worth it for the 26-year-old ad salesman, whose girlfriend also routinely relies on telehealth to see her nutritionist. “It’s a very easy way to get an expert opinion without having to necessarily leave your apartment,” fill out forms or spend idle time in waiting rooms, Freyre says. “We all know what going to the doctor can be like.”But now, Freyre has a sore knee — and he’s not content to to visit his doctor by phone or Zoom. “That’s something that I will 100% want handled in person.”
The $20 copay was well worth it for the 26-year-old ad salesman, whose girlfriend also routinely relies on telehealth to see her nutritionist. “It’s a very easy way to get an expert opinion without having to necessarily leave your apartment,” fill out forms or spend idle time in waiting rooms, Freyre says. “We all know what going to the doctor can be like.”But now, Freyre has a sore knee — and he’s not content to to visit his doctor by phone or Zoom. “That’s something that I will 100% want handled in person.”
 “If you boost people who have originally received J&J with either Moderna or Pfizer, the level of antibodies that you induce in them is much higher than if you boost them with the original J&J,” Fauci told reporters during a television interview.
“If you boost people who have originally received J&J with either Moderna or Pfizer, the level of antibodies that you induce in them is much higher than if you boost them with the original J&J,” Fauci told reporters during a television interview.
 A highly anticipated study of “mixing and matching” Covid-19 vaccines found the approach to be safe and effective, although the Moderna and Pfizer-BioNTech vaccines were found to spark stronger immune system responses than Johnson & Johnson’s vaccine. “Mixing and matching” refers to giving a booster dose of a vaccine different from the vaccine type that was used for the initial vaccination series.
A highly anticipated study of “mixing and matching” Covid-19 vaccines found the approach to be safe and effective, although the Moderna and Pfizer-BioNTech vaccines were found to spark stronger immune system responses than Johnson & Johnson’s vaccine. “Mixing and matching” refers to giving a booster dose of a vaccine different from the vaccine type that was used for the initial vaccination series.
 ICC’s 18th annual gala was held virtually for the second time, in keeping with Covid-19 safety protocols, which discourage gatherings of large groups indoors. A friendly-but-competitive live auction, followed by a lively pledge drive, quickly raised more than $257,000 to support the community center, a second home to many Indian American seniors and youth. “J&J, BioNTech, and Moderna had never created vaccines before. But everyone saw the public health crisis that was happening — as 10,000 people died each day — and wanted to help,” said Mammen, who was interviewed at the gala by Divya Ganesan, a Stanford University freshman, and co-founder of Real Talk Ed.
ICC’s 18th annual gala was held virtually for the second time, in keeping with Covid-19 safety protocols, which discourage gatherings of large groups indoors. A friendly-but-competitive live auction, followed by a lively pledge drive, quickly raised more than $257,000 to support the community center, a second home to many Indian American seniors and youth. “J&J, BioNTech, and Moderna had never created vaccines before. But everyone saw the public health crisis that was happening — as 10,000 people died each day — and wanted to help,” said Mammen, who was interviewed at the gala by Divya Ganesan, a Stanford University freshman, and co-founder of Real Talk Ed.
 The WHO said on Wednesday its recommendation is based on results from more than 2.3 million doses of the vaccine that have been administered to more than 800,000 children in pilot countries Ghana, Kenya and Malawi since 2019, Xinhua news agency reported.
The WHO said on Wednesday its recommendation is based on results from more than 2.3 million doses of the vaccine that have been administered to more than 800,000 children in pilot countries Ghana, Kenya and Malawi since 2019, Xinhua news agency reported.
 Incorporating cutting-edge science on nutrients, food ingredients, processing characteristics, phytochemicals, and additives (existing systems focus largely on just a few nutrients); and Objectively scoring all foods, beverages, and even mixed dishes and meals using one consistent score (existing systems subjectively group and score foods differently). “Once you get beyond ‘eat your veggies, avoid soda,’ the public is pretty confused about how to identify healthier choices in the grocery store, cafeteria, and restaurant,” said the study’s lead and corresponding author,
Incorporating cutting-edge science on nutrients, food ingredients, processing characteristics, phytochemicals, and additives (existing systems focus largely on just a few nutrients); and Objectively scoring all foods, beverages, and even mixed dishes and meals using one consistent score (existing systems subjectively group and score foods differently). “Once you get beyond ‘eat your veggies, avoid soda,’ the public is pretty confused about how to identify healthier choices in the grocery store, cafeteria, and restaurant,” said the study’s lead and corresponding author, 
 “Harnessing the power of Indian Doctors worldwide, the AAPI Global Healthcare Summit platform has evolved with the support of prominent global and Indian medical associations,” says Dr. Anupama Gotimukula, President of AAPI. “The theme for the Summit this year is, ‘Prevention Is Better Than Cure Through Technology, Telemedicine & Transformation’ and we want to coordinate and collaborate all our resources towards helping India emerge stronger and healthier.”
“Harnessing the power of Indian Doctors worldwide, the AAPI Global Healthcare Summit platform has evolved with the support of prominent global and Indian medical associations,” says Dr. Anupama Gotimukula, President of AAPI. “The theme for the Summit this year is, ‘Prevention Is Better Than Cure Through Technology, Telemedicine & Transformation’ and we want to coordinate and collaborate all our resources towards helping India emerge stronger and healthier.” “Physicians and delegates from different parts of the world will come together, facilitating exchange of knowledge, cutting edge technology and best practices in protecting and promoting healthcare,” Dr. Udaya Shivangi, Chair of AAPI GHS USA 2021 says. “In addition to continuing the ongoing projects commenced by past AAPI leaders, GHS will have new initiatives and innovative ideas. The GHS 2022 will focus on envisioning future digital health solutions, and preventive strategies with state of the art CMEs and Symposiums with information on current and emerging issues and trends in healthcare.”While elaborating on the themes and areas that are going to be covered during the Summit, Dr. Kusum Punjabi, Chair of AAPI BOT, says, “In our efforts to realize the core mission of AAPI, which is to share the best from leading experts from around the world, to collaborate on clinical challenges, research and development, philanthropy, policy and standards formulation, the Summit in Hyderabad will have clinical tracks that are of vital to healthcare in India.”
“Physicians and delegates from different parts of the world will come together, facilitating exchange of knowledge, cutting edge technology and best practices in protecting and promoting healthcare,” Dr. Udaya Shivangi, Chair of AAPI GHS USA 2021 says. “In addition to continuing the ongoing projects commenced by past AAPI leaders, GHS will have new initiatives and innovative ideas. The GHS 2022 will focus on envisioning future digital health solutions, and preventive strategies with state of the art CMEs and Symposiums with information on current and emerging issues and trends in healthcare.”While elaborating on the themes and areas that are going to be covered during the Summit, Dr. Kusum Punjabi, Chair of AAPI BOT, says, “In our efforts to realize the core mission of AAPI, which is to share the best from leading experts from around the world, to collaborate on clinical challenges, research and development, philanthropy, policy and standards formulation, the Summit in Hyderabad will have clinical tracks that are of vital to healthcare in India.”
 These findings,
These findings, 
 Health experts say the fourth wave of the pandemic has peaked overall in the U.S., particularly in the Deep South, where hospitals were stretched to the limit weeks ago. But many Northern states are still struggling with rising cases, and what’s ahead for winter is far less clear. Unknowns include how flu season may strain already depleted hospital staffs and whether those who have refused to get vaccinated will change their minds.
Health experts say the fourth wave of the pandemic has peaked overall in the U.S., particularly in the Deep South, where hospitals were stretched to the limit weeks ago. But many Northern states are still struggling with rising cases, and what’s ahead for winter is far less clear. Unknowns include how flu season may strain already depleted hospital staffs and whether those who have refused to get vaccinated will change their minds.
 It found that about 36% of Covid patients still reported disease symptoms three and six months after diagnosis. Most previous studies estimated the so-called long-haul Covid to afflict 10% to 30% of patients. The researchers also found that of those who had long COVID three to six months after diagnosis, roughly 40% had no record of such symptoms in the prior three months.
It found that about 36% of Covid patients still reported disease symptoms three and six months after diagnosis. Most previous studies estimated the so-called long-haul Covid to afflict 10% to 30% of patients. The researchers also found that of those who had long COVID three to six months after diagnosis, roughly 40% had no record of such symptoms in the prior three months.
 What is the unique health ID, and how does one get it?
What is the unique health ID, and how does one get it?
 In the course of the COVID-19 pandemic, thousands of variants have been identified, four of which are considered “
In the course of the COVID-19 pandemic, thousands of variants have been identified, four of which are considered “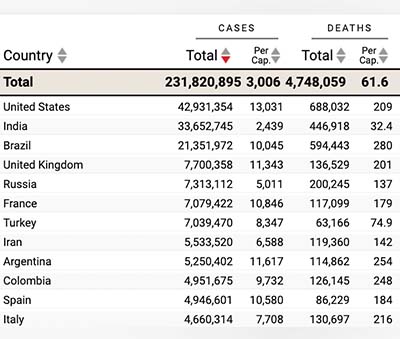 Coronaviruses more prone to mutations than other germs
Coronaviruses more prone to mutations than other germs

 The Governor of Sikkim, Ganga Prasad, praised the foundation initiative and congratulated all the awardees. He launched the stickers, “I Salute Doctors”, in the presence of all the dignitaries. He said Nisha foundation is working towards a wonderful mission for betterment of society. Kulstey said Nisha foundation initiative is great and he applaud this program and appreciated Nisha foundation for working in 173 countries in association of world Organization of peace for child education, sports and salutation evening in name of frontliners During his speech he said it’s important to do this kind of programs to uplift human consciousness and he expressed his concern for farmers.
The Governor of Sikkim, Ganga Prasad, praised the foundation initiative and congratulated all the awardees. He launched the stickers, “I Salute Doctors”, in the presence of all the dignitaries. He said Nisha foundation is working towards a wonderful mission for betterment of society. Kulstey said Nisha foundation initiative is great and he applaud this program and appreciated Nisha foundation for working in 173 countries in association of world Organization of peace for child education, sports and salutation evening in name of frontliners During his speech he said it’s important to do this kind of programs to uplift human consciousness and he expressed his concern for farmers.