“Corruption, embezzlement, fraud are all characteristics which exist everywhere. It is regrettably how human nature functions, whether we like it or not. What successful economies do is keep it to a minimum. But, unfortunately, no one has ever eliminated any of that stuff”- said. Alan Greenspan, on the evil characteristic of frauds in general.
In USA, the system of Medicare benefits has been an abundant resource for fraudsters. Medicare improper payments were estimated to be $25.74 billion in fiscal year 2020. However, the amount of improper payments made in Medicare are significant, during 2019 representing to an amount of $28.91 billion.
Medicare fraud occurs when someone, whether doctors or patients or scammers, knowingly deceives Medicare to receive payment when they receive a higher payment than they should. Committing fraud is illegal and should be reported. Anyone can commit or be involved in fraud, and there are cases of fraudsters including doctors, other providers, and Medicare beneficiaries.
 Some common examples of Medicare fraud include billing for services that were not provided, over billing, billing unnecessary services, misrepresenting dates of service or providers of service, and paying kickbacks for patient referrals.
Some common examples of Medicare fraud include billing for services that were not provided, over billing, billing unnecessary services, misrepresenting dates of service or providers of service, and paying kickbacks for patient referrals.
Medicare fraud happens when someone illegally use their Medicare card to get medical care, supplies, or equipment, or sell their Medicare number to someone who bills Medicare for services not received, or provide their Medicare number in exchange for money or a gift.
But sporadic instances of frauds are committed by greedy doctors, and a recent case reported, unveils an example of similar cases.
Ravi Murali, 39, formerly from Wisconsin, was sentenced by Chief U.S. District Judge James D. Peterson to 54 months in federal prison for Dr. Murali’s role in defraud Medicare. He pleaded guilty to this charge on March 31, 2021.
Dr. Murali wrote thousands of fraudulent orders for Durable Medical Equipment (DME). Other participants in the scheme used Dr. Murali’s fraudulent orders to bill Medicare $26,000,000, of which Medicare paid $13,000,000.
As we all know, Medicare is complicated. What may seem like an error to the beneficiary, may result from a misunderstanding about benefits.
It may also be abuse, which involves billing Medicare for services that are not covered or are not correctly coded. The provider has not knowingly and intentionally misrepresented the facts to obtain payment.
Medicare fraud assumes criminal offense. The Centers for Medicare and Medicaid Services (CMS) defines fraud as “the intentional deception or misrepresentation that the individual knows to be false or does not believe to be true,” and that is made “knowing that the deception could result in some unauthorized benefit to themselves or some other person.
Some common examples of suspected Medicare fraud or abuse are:
- Billing for services or supplies that were not provided
- Providing unsolicited supplies to beneficiaries
- Misrepresenting a diagnosis, a beneficiary’s identity, the service provided, or other facts to justify payment
- Prescribing or providing excessive or unnecessary tests and services
- Violating the participating provider agreement with Medicare by refusing to bill Medicare for covered services or items and billing the beneficiary instead
- Offering or receiving a kickback (bribe) in exchange for a beneficiary’s Medicare number
- Requesting Medicare numbers at an educational presentation or in an unsolicited phone call
- Routinely waiving co-insurance to attract business
The federal government has made significant strides in reducing fraud, waste, and improper payments across the government.
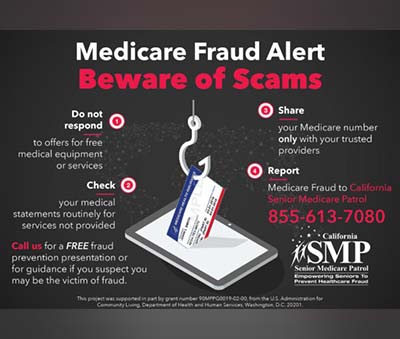
The CMS “Guard Your Card” campaign tells people how they can protect themselves against fraud by:
- Never give out their Medicare or Social Security Number to anyone except those you know should have it.
- They reported any suspicious activities like being asked over the phone for their Medicare/Social Security number or banking information. Medicare will NEVER call you uninvited for this information.
- By checking their billing statements and reporting suspicious charges. Using a calendar to track doctor’s appointments and services helps quickly spot possible fraud and billing mistakes. Check claims early by logging into gov.
Any suspicious activities may be reported by calling 1-800-MEDICARE (1-800-633-4227).
Under the False Claims Act (FCA), the government may pay a reward of up to 30% to people who report healthcare fraud. In September 2019, TELG client Kevin Manieri was awarded more than $12 million for reporting that a drug company defrauded Medicare and other government insurance programs by encouraging doctors to prescribe an unnecessary medication to patients.
Health care fraud is a felony under Michigan’s Health Care False Claims Act, punishable by up to four years in prison, a $50,000 fine and loss of health insurance. It’s also a federal criminal offense under the Health Insurance Portability and Accountability Act.











