Even though people are becoming more connected through social media and other outlets, the great irony is that many people still feel lonely. That loneliness, in turn, can have far-reaching implications on a person’s health and well-being. Loneliness as a public health issue has been intensified during the COVID-19 pandemic. Knowing how to recognize loneliness and what can help patients overcome feeling lonely is key.
There’s a gap in feeling connected
“Loneliness is essentially the feeling of being uncomfortable or in distress when someone feels that there is a gap between the connection they would like and the connection they actually have,” said Dr. Bell Washington, adding that “you can be in a crowd full of people, you can know all of them, and you can still feel lonely.”
“So, you might have a lot of superficial social connections, but what you really want is something deeper—someone to know you on the inside,” she said. “It’s really based on perception of the difference between the relationship you’d like and the relationship that you have with others.”
Younger people are feeling lonelier
“Loneliness was already an epidemic of its own, but the global COVID-19 pandemic caused loneliness to increase substantially over the past few years,” said Dr. Bell Washington, who took a course during the last year of her MPH program at Harvard T.H. Chan School of Public Medicine where she learned the serious complications of loneliness. “A 2021 online survey found that 36% of all Americans—which includes 61% of young adults and 51% of mothers with young children—feel ’serious loneliness.’”
Additionally, the Centers for Disease Control and Prevention (CDC) “found 63% of young adults also suffer significant symptoms of anxiety or depression,” she said. “That means we have a generation of young people hungry for deeper connection who often do not have the skills or opportunities to achieve it.”
“One’s 20s are filled with countless social expectations including separating from one’s nuclear family, finding a partner, developing a career and finding a ‘tribe,’” Dr. Bell Washington said. “For many this time is complicated by unrealistic social media lives which are often unattainable. That only amplifies the loneliness that young adults feel.”
Social isolation can play a role
“An individual experiencing loneliness will often describe feeling alone. This is distinct from social isolation where there is a paucity of social connectedness,” said Dr. Clark. “Social isolation can be a sequela of loneliness, but there are plenty of individuals who experience loneliness and are still socially connected.”
Additionally, “there are some people who I would consider socially isolated, but they feel perfectly fine with it,” said Dr. Bell Washington. “The pandemic revealed that though some people considered themselves loners, when they truly had to be alone all of the time (due to quarantine or isolation), they found out that they actually do value social connection, and would have preferred to be with other people.”
Social media affects loneliness
“We get these dopamine surges when someone likes our status,” said Dr. Clark, referring to a social media posting. Many, conversely, feel “sad or upset when they do not receive a certain number of likes or have over 1 million followers on their social media accounts.
“And if you’re having an identity crisis—and if you’re letting social media dictate who you are—that can create some loneliness,” he added. “We must be mindful of the psychiatric sequelae of loneliness. These include depression and anxiety.”
Everyone is at risk for loneliness
“We’re all at risk for loneliness in our lives,” said Dr. Clark. “There was a report that came out from the National Academies of Science, Engineering and Medicine. It revealed that more than one-third of adults 45 or older reported feeling lonely and about a quarter of adults 65 or older were considered to be socially isolated.
“Social isolation in itself was associated with a 50% increased risk of developing a neurocognitive disorder and other serious medical conditions,” he added. “No one is immune to loneliness and social isolation, but there are certain groups who are at increased risk.”
“When we think about historically marginalized groups in terms of immigrants—as well as the LGBTQ+ community—those are groups that have been shown to be at high risk for loneliness and social isolation,” Dr. Clark said.
“Anyone can suffer from loneliness and the highest risk is for those who are not able to remedy the loneliness when they feel it,” Dr. Bell Washington echoed. She added, “The fear of being alone in your loneliness only makes the isolation worse. It is easy to feel you’re the only one who needs social connectedness, but that is not true. There is no shame in being lonely. We were built for connection.”
It’s linked to health complications
“There is some evidence to note that people who are experiencing social isolation and loneliness are at increased risk for premature death,” said Dr. Clark, adding that “social isolation and loneliness were associated with a 29% increased risk of heart disease and a 32% risk of stroke.”
“Now, I’m a romantic and a poet, and there’s something to be said about the broken heart—literally and figuratively speaking,” he said. “If you’re already feeling lonely, that’s going to impact your heart. If you’re feeling socially isolated, that’s going to impact your heart.”
Discrimination is also a factor
Looking at “immigrants and the LGBTQ+ group, why do these groups feel so isolated and lonely? Well, discrimination is a factor that can be a barrier for them being able to feel socially connected,” said Dr. Clark. “The other thing would be language barriers if we’re talking about immigrants where English is not their primary language.”
“It can be difficult to form relationships with others when historically marginalized groups continue to be stigmatized,” he said. “We have to acknowledge our implicit and explicit biases if we hope to seek to embrace humanity in the form of diversity, equity and inclusion.”
Acknowledge how you’re feeling
“Sometimes we are in denial. When we’re in denial, it’s easy to avoid those feelings that we know are bubbling on the surface, but we just try to continue to suppress them,” said Dr. Clark. “If you are feeling lonely, the first thing is, acknowledge that, and then ask yourself: What is contributing to my loneliness?”
“Loneliness is not your fault. Social isolation is not your fault,” he said. “Because, again, there are probably precipitating and perpetuating factors that are contributing to these states of being.”
“We have to remember that we are enough and that we belong,” Dr. Clark said.
Related Coverage
What doctors wish patients knew about family immunizations
Everyone needs a support system
“If we’re wanting people to live longer, healthier lives, we have to be better about investigating how loneliness is impacting our communities,” said Dr. Clark. “Everybody needs a support system. Even the person who says that they have a shy temperament and they’re more introverted—they still need a support system.” “When we’re looking at our AMA declaring this as a public health issue, it speaks to the importance of advocating for connectedness for all communities that will enable them to flourish,” he said. “For example, supports systems are a positive, prognostic factor for individuals who are suffering from mental health conditions, substance-use disorders and personality disorders.”
“We have to make sure people have the available resources that will allow them to cultivate connectedness,” Dr. Clark said, adding that “these resources must be diverse, equitable and inclusive.”
Don’t minimize anyone’s struggle
“People assume if someone is doing well, making money and has a family that they can’t be lonely, but that is not true,” said Dr. Bell Washington. “We all benefit from having a deeper connection with others, no matter what stage of life we’re in.”
“We really can’t minimize anyone’s struggle, because we all have different difficulties that we’re coping with,” she said. “We are human, we have needs and we have a right to express those needs. We should always be kinder than necessary because you never know the hidden battles that people are going through.”
Take loneliness seriously
“Loneliness is something to be taken seriously,” said Dr. Bell Washington. Loneliness “can have serious mental and physical complications that worsen if ignored.” She added that, “social isolation and loneliness lead to higher risk of high blood pressure, heart disease, obesity, anxiety, depression, memory issues and even death.”
“It is not a sign of weakness. You do not have to be a superhero. You don’t have to be strong all of the time and there’s nothing wrong with desiring or seeking connections,” she said. “The same things we needed as little kids; we need as adults too. So, of course you need sleep, healthy food and physical activity, but you also need connection.”
“That connection looks different for different people. For some, it may be connection with a higher power, family or friends,” Dr. Bell Washington said. “I advise all patients to make sure you are taking care of yourself and seek help if you need it.” Washington
Reach out to your physician for help
“If you notice that you are sad or worried more days than not, that would be a sign that you probably should check in with someone,” said Dr. Bell Washington. “In addition to confiding in a trusted family friend, I’d recommend reaching out to your personal physician.
“They can make sure you are not suffering from depression or other mood issues as a result of your loneliness,” she added. “Your doctor would be a great person because they can be sure to provide you some help as well.”
“Then obviously if you get to the point where you’re feeling so lonely and so isolated that you start feeling hopeless or suicidal, you should reach out to your doctor immediately,” Dr. Bell Washington said, noting “there’s also a new 988 mental health hotline. Whatever you do, don’t suffer in silence, please get help!”
(Two psychiatrists, AMA members share their thoughts on what patients need to know about loneliness as a public health issue. These AMA members are:
- Tiffani Bell Washington, MD, MPH, an outpatient general, child and adolescent psychiatrist working with Centurion and also in private practice in North Carolina. She is an American Psychiatric Association delegate to the AMA Young Physicians Section, alternate delegate to the Section Council on Psychiatry and a member of the AMA Ambassador Program, which equips individuals with the skills and knowledge to confidently speak to the AMA’s initiatives and the value of AMA membership.
- Frank Clark, MD, an adult outpatient psychiatrist at Prisma Health in Greenville, South Carolina, and associate clinical professor at the University of South Carolina School of Medicine-Greenville. He is also an American Psychiatric Association delegate to the AMA Section Council on Psychiatry.)
Courtesy: https://www.ama-assn.org/delivering-care/public-health/what-doctors-wish-patients-knew-about-loneliness-and-health?utm_source=BulletinHealthCare&utm_medium=email&utm_term=091022&utm_content=physicians&utm_campaign=article_alert-morning_rounds_weekend

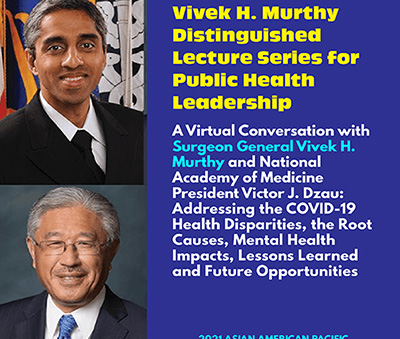 But “I also worry about what’s happened to our clinicians. Yes, they have been absolute heroes, but that’s coming at a cost,” said Dr. Murthy. “The question that we have to ask ourselves as a country is: Are we willing to finally step up and do something?
But “I also worry about what’s happened to our clinicians. Yes, they have been absolute heroes, but that’s coming at a cost,” said Dr. Murthy. “The question that we have to ask ourselves as a country is: Are we willing to finally step up and do something?