The first ever World Health Congress organized by the American Association of Physicians of Indian origin (AAPI) held from July 18-22nd, 2024 came to a close here at the Marriott Marquis on Times Square in New York City with the call by the outgoing President, Dr. Anajana Samadder to work towards the realization of the mission of AAPI.
“I want to thank the AAPI delegates, sponsors and organizing committee who have put together such a great event at the heart of New York City,” Dr. Samadder said in her concluding address. “We have had an exciting 1st ever World Health Congress that was full of fun-filled, educational and entertaining. There was something for everyone, including the younger generation, the teenagers, and children, as wells to the AAPI members, making it a family event,” said Dr. Samadder.
 In her keynote address at the gala on Sunday night, Honorable Smriti Irani, a former Cabinet Minister of India and a Bollywood star shared with the over 1,500 AAPI delegates who came from across the United States about the many contributions of India to the world, especially in the healthcare filed and the numerous achievements of the Government of India. She thanked the AAPI members for their great contributions and services to the people of the United States and for their motherland India.
In her keynote address at the gala on Sunday night, Honorable Smriti Irani, a former Cabinet Minister of India and a Bollywood star shared with the over 1,500 AAPI delegates who came from across the United States about the many contributions of India to the world, especially in the healthcare filed and the numerous achievements of the Government of India. She thanked the AAPI members for their great contributions and services to the people of the United States and for their motherland India.
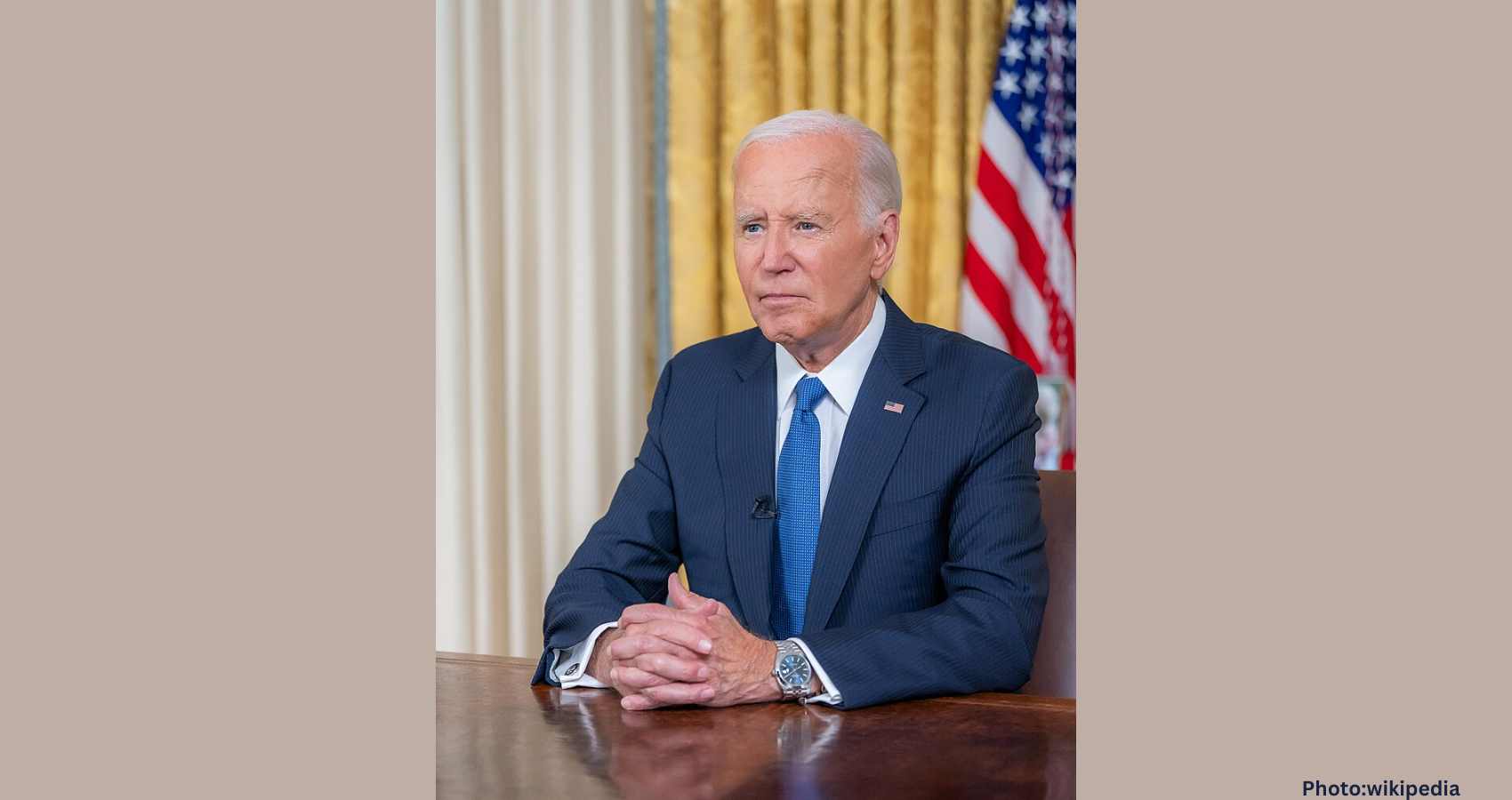
The World Health Congress, which began on July 18th with the cutting of the Ribbon by the Mayor of New York City, Eric Adams is being attended by over 1,000 physicians and has over 80 speakers and CEOs from around the globe, provide the delegates with an unparalleled opportunity to network, learn, and explore groundbreaking advancements across healthcare disciplines.
Some of the key speakers addressed the delegates at the Congress included: Dr. Mehmet Oz, American television personality, Physician, Author, and Professor Emeritus of cardiothoracic surgery at Columbia University; Eric Adamas, Mayor of New York City; Smriti Zubin Irani, an Indian politician and former actress, fashion model, and television producer; Binaya Srikanta Pradhan, Consul General of India in New York, Dilip Chauhan, Deputy Commissioner for Trade, Investment and Innovation, and NY Assembly woman Jenifer Rajkumar.
 New York City Mayor Eric Adams inaugurated the World Health Congress of Physicians with the cutting of the Ribbon and a powerful and memorable inaugural address on July 18th, 2024. In his inaugural address, Adams lauded the contributions of Indian American physicians across the United States, especially during the Covid pandemic. “When you look at the 1000s of physicians across the country, you walk into any hospital, the emergency rooms, especially during COVID, you were present. You were there, and you sacrificed your own health to make sure of the health of this entire country. Your contributions are so rare.”
New York City Mayor Eric Adams inaugurated the World Health Congress of Physicians with the cutting of the Ribbon and a powerful and memorable inaugural address on July 18th, 2024. In his inaugural address, Adams lauded the contributions of Indian American physicians across the United States, especially during the Covid pandemic. “When you look at the 1000s of physicians across the country, you walk into any hospital, the emergency rooms, especially during COVID, you were present. You were there, and you sacrificed your own health to make sure of the health of this entire country. Your contributions are so rare.”
Dr. Mehmet Oz delivered an inspiring talk on “Living the Good Life” sharing with delegates who had assembled at the Broadway Ballroom his insights into wellness and health optimization that resonate deeply within and beyond the medical community.
Sri Brahmrishi SiddhGuru Gurudev, while bestowing his blessings on the organizers and the AAPI delegates called the Indian American Physicians “the best” in the world, because “they give their best to the world.” He lauded them for their virtues of “learning, earning and returning” that makes them stand out across the globe.

Pramukh Swami Dr. Swami Gyanvatsal, a Motivational Speaker from Akshardham, BAPS Swaminaryan Mandir presented his inspirational talk on “Physician Burnout.” Swami Gyanvasti Dr. Gyan Vatsal focused on various aspects of personal development, spirituality, social harmony, giving back to society, education, and knowledge, highlighting the significance of continuous learning and education in personal growth.
The CEO Forum was moderated by Dr. Achintya Moulick, Chair of the AAPI World Health Congress. In his opening remarks, Dr. Moulick said, “The first World Congress of AAPI signals the beginning of a new chapter for the organization which has had a significant impact on American healthcare. The goal for me as the first convention chair of the World Congress is to bring healthcare providers, entrepreneurs, financial bodies and policymakers together and create a perfect gathering of first, second and third generation physicians and other healthcare providers of Indian origin lead the way for the future of global health.”
The CEO had industry leaders from healthcare, pharma and IT, including Dr. Oz; Edward Chan, 1315 Capitall; Michael Kopko,, Co-founder & CEO | Pearl Health; Hemanth Neeli,, Inhospital Physicians; Ishan Shivanand,, Yoga of Immortals (YOI); and Dr. Samin Sharma, The Mount Sinai Hospital, Director, Cardiovascular Clinical Institute. The inspiration forum deliberated on ways to provide the best and most efficient healthcare delivery to patients, with minimum cost and how AI has and will influence healthcare delivery in the US and around the world.

AAPI’s Legislative Day discussed the need to regulate healthcare, visa, physician-patient relationship, insurance issues and was moderated by Dr. Sumul Raval, national Secretary of AAPI. He said, “AAPI’s lobbying efforts on some of the issues affecting the broader Indian American community and other immigrant groups is also a testament to its growth and reach. Being one of the oldest Indian American organizations, it’s also among the most influential, as was evident from the lawmakers who took time out of their busy schedule to address the group.”
Dr. Srinagesh Paluvoi, member of AAPI’s national Board of Trustees, and the Regional Director, Mid Atlantic-I Region Dr. Bhavani Srinivasan moderated the Legislative Day. Lawmakers how were part of the Panel included: New York City Councilwoman Susan Zhuang; New York City Councilman Shekar Krishnan; NY Assemblywoman Jenifer Rajkumarl; Ravi Reddi, representing the Office of US Senator Kirsten Gillibrand; New Jersey state Senator Vin Gopal; and, NYC Councilwoman Majority Whip Selvena N. Brooks-Powers. During the discussions, AAPI members highlighted the importance of healthcare delivery, Green Card backlog, physician-patient health relationship, and insurance issues. In a show of support for AAPI, all the lawmakers addressed the AAPI delegates and listened to their concerns and promised support.
Moderated by Dr. Bhavani Srinivasan and co-moderated by Dr. Mamta Singhvi co moderator, past president of MSRF and led by Dr. Anjana Samadder, president of AAPI, the popular Women’s Forum had Smiriti Irani, former federal Minister from India and Bollywood star, Dr. Leena Gupta, Regional Director from the West Coast, Yoshita Singh, Press Trust of India, Chief Correspondent for USA and the United Nations, Dr. Soumya Vishvanathan, a physician and corporate leader, leading a group of 17 Hospitals in Florida. Each of them shared with the audience their personal journey to become successful in their professional careers.
 Some of the major themes at the convention include: Yoga and Meditation practices, a welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, yoga therapy sessions, a workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine, and several wellness sessions.
Some of the major themes at the convention include: Yoga and Meditation practices, a welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, yoga therapy sessions, a workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine, and several wellness sessions.
The World Congress has had, among many others, sessions on cutting-edge research and CMEs, promoting business relationships, and displaying of ethnic items. Artificial Intelligence (AI) was the prime focus of our World Health Congress. There were entertainment features for children, live and exciting performances by Javed Ali and Atif Aslam, Aditya Narayan, Traditional Garba, Bollywood Film Festival, a standup comedy show by Kapil Sharma and a fashion show by the world renowned fashion designer and artist Archana Kochar.
In addition to colorful entertainment, and exquisite authentic Indian cuisine, esteemed health industry leaders, world-renowned speakers, and experts shared their wisdom and expertise in the industry, offering enlightening sessions to the delegates.
AAPI’s World Health Congress offered an exciting venue to interact with leading physicians, health professionals, academicians, and scientists of Indian origin. The physicians and healthcare professionals from across the country will convene and participate in the scholarly exchange of medical advances, to develop health policy agendas, and to encourage legislative priorities in the coming year.
 Amit Chakrabarty, Vice President of AAPI said, “AAPI’s mission has evolved in the past 42 years. “Today, AAPI is strong representing over 120,000 Indian American physicians, 130 local Chapters, who make up 10% of total physicians in the US and nearly 50% of International Medical Graduates, rooted in every corner of the nation, who serve every 7th patient in the US. We are proud of our achievements and our contributions to the healthcare industry and the millions of people we serve.”
Amit Chakrabarty, Vice President of AAPI said, “AAPI’s mission has evolved in the past 42 years. “Today, AAPI is strong representing over 120,000 Indian American physicians, 130 local Chapters, who make up 10% of total physicians in the US and nearly 50% of International Medical Graduates, rooted in every corner of the nation, who serve every 7th patient in the US. We are proud of our achievements and our contributions to the healthcare industry and the millions of people we serve.”
Dr. Lokesh Edara, Chair, AAPI Board of Trustees said, “The growing influence of doctors of Indian heritage is evident, as increasingly physicians of Indian origin hold critical positions in the healthcare, academic, research and administrative positions across the nation. With their hard work, dedication, compassion, and skills, they have thus carved an enviable niche in the American medical community. AAPI’s role has come to be recognized as vital among members and among lawmakers.”
 Research and Arts Competition: Poster Competition brought in the best among the aspiring medical students and new graduates from Medical schools. A Panel Discussion on Global Medical Education addressed by the Heads of NBME, FSMB, Intealth, NBME, and NBEMS offered practical tools on navigating the educational systems across India, UK and the United States.
Research and Arts Competition: Poster Competition brought in the best among the aspiring medical students and new graduates from Medical schools. A Panel Discussion on Global Medical Education addressed by the Heads of NBME, FSMB, Intealth, NBME, and NBEMS offered practical tools on navigating the educational systems across India, UK and the United States.
Networking Mixer and Speed dating was a unique session catering to the needs of the young physician community. Immigration Talk by Nalini Mahadevan provided insights into current immigration trends and about the ways to obtain Resident/Green Card status to physicians community members.
Can India become a Vishwaguru in Healthcare? by Dr. Anupam Sibal was an important topic that provided insights into how India is becoming a world leader in Medicine.
 Each day began for the participants with an hour long session on “Harmony and Health: Integrative Yoga” where delegates benefited from hands on sessions teaching and practicing Yoga. Another theme that ran across all days of the Congress was Art Gallery – Oorja: The Feminine Light in Indian Art. Healing Breath that was part of the schedule everyday of the Congress was another way AAPI delegates had an opportunity to ground themselves to the present and start afresh.
Each day began for the participants with an hour long session on “Harmony and Health: Integrative Yoga” where delegates benefited from hands on sessions teaching and practicing Yoga. Another theme that ran across all days of the Congress was Art Gallery – Oorja: The Feminine Light in Indian Art. Healing Breath that was part of the schedule everyday of the Congress was another way AAPI delegates had an opportunity to ground themselves to the present and start afresh.
Cultural Programs including “AAPI GOT TALENT” offered an opportunity to Physicians to showcase their talents in art and music, competing with one another for top honors.
Making it relevant and meaningful to young children, each day had a session on “Sky Kids and Sky Teens Leadership Camp” providing them with meaningful insights on self-development. Bollywood Bhangra workout LIVE by Zumbhangra was another way offered to members to relax and learn new ways to stress reduction.
 The growing influence of doctors of Indian heritage is evident, as increasingly physicians of Indian origin hold critical positions in the healthcare, academic, research and administrative positions across the nation. With their hard work, dedication, compassion, and skills, they have thus carved an enviable niche in the American medical community. AAPI’s role has come to be recognized as vital among members and among lawmakers.
The growing influence of doctors of Indian heritage is evident, as increasingly physicians of Indian origin hold critical positions in the healthcare, academic, research and administrative positions across the nation. With their hard work, dedication, compassion, and skills, they have thus carved an enviable niche in the American medical community. AAPI’s role has come to be recognized as vital among members and among lawmakers.
“The 1st ever World Congress of AAPI has offered extensive academic presentations, recognition of achievements and achievers, and professional networking at the alumni and evening social events,” said Dr. Samadder, whose one-year term as AAPI president has come to a close as per AAPI bylaws. For more details on AAPI and the 1st World Congress, please visit: www.aapiusa.org






 As the President-Elect, the multi-talented professional said, “I understand that AAPI needs experienced leadership from someone who has been in AAPI leadership for over two decades. I know what works and what does not. This is a major contribution that I can make this year in guiding the leadership to progress in the right direction efficiently and effectively.”
As the President-Elect, the multi-talented professional said, “I understand that AAPI needs experienced leadership from someone who has been in AAPI leadership for over two decades. I know what works and what does not. This is a major contribution that I can make this year in guiding the leadership to progress in the right direction efficiently and effectively.” clinical professor of medicine at Wright State University-Boonshoft School of Medicine, Dayton, Ohio. Dr. Kathula is a Diplomate of the American Board of Lifestyle Medicine. He has authored several papers and articles in medical journals and is in the process of writing a book, describing his journey as an immigrant physician. “For the past 22 years, I’ve been proudly serving as a Hematologist and Oncologist in the Dayton community, considering it my home:”
clinical professor of medicine at Wright State University-Boonshoft School of Medicine, Dayton, Ohio. Dr. Kathula is a Diplomate of the American Board of Lifestyle Medicine. He has authored several papers and articles in medical journals and is in the process of writing a book, describing his journey as an immigrant physician. “For the past 22 years, I’ve been proudly serving as a Hematologist and Oncologist in the Dayton community, considering it my home:” The growing influence of physicians of Indian heritage is evident, as increasingly physicians of Indian origin hold critical positions in healthcare, academic, research, and administrative positions across the nation. Physicians of Indian origin are known for their great achievements, and their contributions to their motherland, India, and their adopted land, the United States in significant ways to the transformation of Indo-US relations.
The growing influence of physicians of Indian heritage is evident, as increasingly physicians of Indian origin hold critical positions in healthcare, academic, research, and administrative positions across the nation. Physicians of Indian origin are known for their great achievements, and their contributions to their motherland, India, and their adopted land, the United States in significant ways to the transformation of Indo-US relations. In her keynote address at the gala on Sunday night, Honorable Smriti Irani, a former Cabinet Minister of India and a Bollywood star shared with the over 1,500 AAPI delegates who came from across the United States about the many contributions of India to the world, especially in the healthcare filed and the numerous achievements of the Government of India. She thanked the AAPI members for their great contributions and services to the people of the United States and for their motherland India.
In her keynote address at the gala on Sunday night, Honorable Smriti Irani, a former Cabinet Minister of India and a Bollywood star shared with the over 1,500 AAPI delegates who came from across the United States about the many contributions of India to the world, especially in the healthcare filed and the numerous achievements of the Government of India. She thanked the AAPI members for their great contributions and services to the people of the United States and for their motherland India. New York City Mayor Eric Adams inaugurated the World Health Congress of Physicians with the cutting of the Ribbon and a powerful and memorable inaugural address on July 18th, 2024. In his inaugural address, Adams lauded the contributions of Indian American physicians across the United States, especially during the Covid pandemic. “When you look at the 1000s of physicians across the country, you walk into any hospital, the emergency rooms, especially during COVID, you were present. You were there, and you sacrificed your own health to make sure of the health of this entire country. Your contributions are so rare.”
New York City Mayor Eric Adams inaugurated the World Health Congress of Physicians with the cutting of the Ribbon and a powerful and memorable inaugural address on July 18th, 2024. In his inaugural address, Adams lauded the contributions of Indian American physicians across the United States, especially during the Covid pandemic. “When you look at the 1000s of physicians across the country, you walk into any hospital, the emergency rooms, especially during COVID, you were present. You were there, and you sacrificed your own health to make sure of the health of this entire country. Your contributions are so rare.”

 Some of the major themes at the convention include: Yoga and Meditation practices, a welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, yoga therapy sessions, a workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine, and several wellness sessions.
Some of the major themes at the convention include: Yoga and Meditation practices, a welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, yoga therapy sessions, a workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine, and several wellness sessions. Amit Chakrabarty, Vice President of AAPI said, “AAPI’s mission has evolved in the past 42 years. “Today, AAPI is strong representing over 120,000 Indian American physicians, 130 local Chapters, who make up 10% of total physicians in the US and nearly 50% of International Medical Graduates, rooted in every corner of the nation, who serve every 7th patient in the US. We are proud of our achievements and our contributions to the healthcare industry and the millions of people we serve.”
Amit Chakrabarty, Vice President of AAPI said, “AAPI’s mission has evolved in the past 42 years. “Today, AAPI is strong representing over 120,000 Indian American physicians, 130 local Chapters, who make up 10% of total physicians in the US and nearly 50% of International Medical Graduates, rooted in every corner of the nation, who serve every 7th patient in the US. We are proud of our achievements and our contributions to the healthcare industry and the millions of people we serve.” Research and Arts Competition: Poster Competition brought in the best among the aspiring medical students and new graduates from Medical schools. A Panel Discussion on Global Medical Education addressed by the Heads of NBME, FSMB, Intealth, NBME, and NBEMS offered practical tools on navigating the educational systems across India, UK and the United States.
Research and Arts Competition: Poster Competition brought in the best among the aspiring medical students and new graduates from Medical schools. A Panel Discussion on Global Medical Education addressed by the Heads of NBME, FSMB, Intealth, NBME, and NBEMS offered practical tools on navigating the educational systems across India, UK and the United States. Each day began for the participants with an hour long session on “Harmony and Health: Integrative Yoga” where delegates benefited from hands on sessions teaching and practicing Yoga. Another theme that ran across all days of the Congress was Art Gallery – Oorja: The Feminine Light in Indian Art. Healing Breath that was part of the schedule everyday of the Congress was another way AAPI delegates had an opportunity to ground themselves to the present and start afresh.
Each day began for the participants with an hour long session on “Harmony and Health: Integrative Yoga” where delegates benefited from hands on sessions teaching and practicing Yoga. Another theme that ran across all days of the Congress was Art Gallery – Oorja: The Feminine Light in Indian Art. Healing Breath that was part of the schedule everyday of the Congress was another way AAPI delegates had an opportunity to ground themselves to the present and start afresh. The growing influence of doctors of Indian heritage is evident, as increasingly physicians of Indian origin hold critical positions in the healthcare, academic, research and administrative positions across the nation. With their hard work, dedication, compassion, and skills, they have thus carved an enviable niche in the American medical community. AAPI’s role has come to be recognized as vital among members and among lawmakers.
The growing influence of doctors of Indian heritage is evident, as increasingly physicians of Indian origin hold critical positions in the healthcare, academic, research and administrative positions across the nation. With their hard work, dedication, compassion, and skills, they have thus carved an enviable niche in the American medical community. AAPI’s role has come to be recognized as vital among members and among lawmakers. (Albany, NY – May 23, 2024) Dr. Hari Krishna Shukla, practicing Medicine in Flushing, Queens in New York for nearly four decades, serving thousands of young patients, was bestowed with the New York State Liberty Medal during a solemn ceremony on the New York Senate Floor in Albany, NY on May 15th, 2024.
(Albany, NY – May 23, 2024) Dr. Hari Krishna Shukla, practicing Medicine in Flushing, Queens in New York for nearly four decades, serving thousands of young patients, was bestowed with the New York State Liberty Medal during a solemn ceremony on the New York Senate Floor in Albany, NY on May 15th, 2024.
 While introducing Dr. Seth, Dr. Lokesh Edara, Chairman of AAPI BOT said, “Dr. Seth is the president of NBEMS, who has brought significant contributions to medical education, increase in much needed post graduate seats I n medical education in India, and has encouraged family medicine post graduated and diploma courses,” he said. “ in addition, he has taken CPR awareness initiatives and worked with several healthcare institutions including NMC, Dental, Nursing, Para Medic, whose numbers have reached more than 2 million people as of 2023.”
While introducing Dr. Seth, Dr. Lokesh Edara, Chairman of AAPI BOT said, “Dr. Seth is the president of NBEMS, who has brought significant contributions to medical education, increase in much needed post graduate seats I n medical education in India, and has encouraged family medicine post graduated and diploma courses,” he said. “ in addition, he has taken CPR awareness initiatives and worked with several healthcare institutions including NMC, Dental, Nursing, Para Medic, whose numbers have reached more than 2 million people as of 2023.” Academia, initially in India and then extensively in the UK. He published more than 20 peer reviewed publications in prestigious journals, including in the Annals of Thoracic Surgery, 40 abstract presentations and 40 conference presentations at the British Thoracic Society, World Congress of Brontology, European Respiratory Society and American Thoracic Society. His major research and publications are in the fields of large airway intervention and Sildenafil therapy for patients with pulmonary hypertension.
Academia, initially in India and then extensively in the UK. He published more than 20 peer reviewed publications in prestigious journals, including in the Annals of Thoracic Surgery, 40 abstract presentations and 40 conference presentations at the British Thoracic Society, World Congress of Brontology, European Respiratory Society and American Thoracic Society. His major research and publications are in the fields of large airway intervention and Sildenafil therapy for patients with pulmonary hypertension.
 The FDA panel accepted
The FDA panel accepted