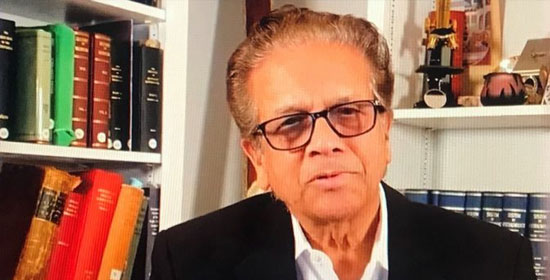
 Rotary’s youth members are joining forces with the globally renowned visionary Dr. V.K. Raju, founder of the Eye Foundation of America (EFA), in a profound mission to eradicate childhood blindness. On June 14, 2025, an inspiring gathering took place at the India International Centre in New Delhi, where a dynamic group of Rotaractors and Interactors expressed their unwavering commitment to carrying forward Dr. Raju’s vision of a “world without childhood blindness.” This event marked a significant step in creating intergenerational partnerships for global health equity.
Rotary’s youth members are joining forces with the globally renowned visionary Dr. V.K. Raju, founder of the Eye Foundation of America (EFA), in a profound mission to eradicate childhood blindness. On June 14, 2025, an inspiring gathering took place at the India International Centre in New Delhi, where a dynamic group of Rotaractors and Interactors expressed their unwavering commitment to carrying forward Dr. Raju’s vision of a “world without childhood blindness.” This event marked a significant step in creating intergenerational partnerships for global health equity.Uniting Passionate Youth Leaders
The event brought together remarkable youth leaders from Rotary’s youth wings, namely Rotaract and Interact clubs. These young changemakers actively contribute to their communities, addressing pressing health and development challenges in alignment with the United Nations Sustainable Development Goals (SDGs).
Key participants in this impactful dialogue included:
· Rotaractor Saacchi Saxena: President of the Rotaract Club of World Without Childhood Blindness and an EFA Youth Ambassador.
· Rotaractor-Rotarian Poorvi Sahai: EFA Ambassador and mentor to the younger generation.
· Interactor Sabyaa Saxena: Immediate Past President of the SDG Community Interact Club and an EFA Young Ambassador.
· Interactor Kaashvi: Current President of the SDG Community Interact Club.
· Interactors Ruhaan and Apal: Student volunteers directly engaged in school-based vision screening campaigns.
These youth leaders, with their passion and dedication, demonstrated how grassroots engagement and collaborative initiatives could serve as the driving force for global change.
The Global Challenge of Childhood Blindness
Childhood blindness remains a significant global health challenge with far-reaching consequences. Dr. Raju highlighted some alarming statistics during his address. For example, three-fourths of children with visual impairments never have the opportunity to attend school. Blindness also significantly reduces employability by up to 50%, which perpetuates cycles of poverty and social isolation.
Dr. Raju specifically drew attention to the situation in India, where approximately 3.5 million premature babies are born annually. Among them, nearly one in six—equivalent to 600,000 infants—are born at less than 32 weeks of gestational age. Of these, about 40% receive neonatal care, and 80% survive, leaving over 200,000 children vulnerable to developing Retinopathy of Prematurity, a preventable cause of childhood blindness.
Strategies and Innovations to Address the Issue
The discussions at the event revolved around scaling the mission of eliminating childhood blindness through grassroots activism, awareness campaigns, and innovative approaches. Some of the key strategies discussed included:
· School-Based Awareness Drives: Empowering students to lead vision screening and educational initiatives within their schools and communities.
· Community Screening Campaigns: Conducting local eye health check-ups to identify and address preventable causes of blindness.
· Technology-Driven Solutions: Leveraging modern tools and digital platforms to enhance the reach and effectiveness of eye care services.
Dr. Raju emphasized the transformative role that Rotary Fellowships could play in building a global network of youth-led initiatives to advance eye health. He shared insights from his vast global experience, illustrating the tangible impact of cohesive action between local and international stakeholders.
Milestones and Future Plans
The meeting also featured several exciting announcements that underscored the commitment of Rotary youth and the Eye Foundation of America:
· Launch of Vision Ambassador Chapters: Schools and colleges will establish these chapters, led by Interactors and Rotaractors, to promote eye health and engage young people in advocacy efforts.
· Global EFA Youth Fellowship: This fellowship will provide training and mentorship to young leaders interested in eye care and public health advocacy.
· #SeeTheFuture Campaign: A powerful youth-led social media movement aimed at raising awareness about childhood blindness and mobilizing global support for the cause.
· Global Vision Summit: Scheduled for January 31, 2027, in New York, this summit will coincide with the proposed International Day for a World Without Childhood Blindness. It will serve as a platform for international dialogue and collaboration.
Each of these milestones represents a concerted effort to institutionalize youth leadership in the fight against childhood blindness while fostering a culture of empathy and action.
Inspiring Words from Dr. Raju
Dr. Raju expressed profound gratitude and admiration for the youth participants, describing them as the leaders of today, not just tomorrow. “If we equip our youth with empathy, purpose, and tools—there is no mission too big, no blindness too deep,” he said. His words resonated deeply with everyone present, reinforcing the belief that young people hold the power to shape a brighter, healthier future.
The event concluded with the signing of a symbolic Charter of Commitments, which outlined the roadmap for future collaborations between Rotary youth clubs, the Eye Foundation of America, and local vision care partners. This charter highlighted the shared goals of preventing childhood blindness, ensuring equitable access to eye care, and empowering every child to see the world clearly.
The collaboration between Rotary youth and Dr. V.K. Raju exemplifies how intergenerational partnerships can address critical global health challenges. By empowering young leaders, fostering innovation, and building alliances, the movement to eradicate childhood blindness is gaining momentum. This monumental effort serves as a testament to the power of compassion, determination, and collective action in shaping a world where every child can see a brighter future.
About the Eye Foundation of America
Founded by Dr. V.K. Raju, the Eye Foundation of America is a global non-profit organization dedicated to preventing blindness through service, education, and research. Over the years, EFA has impacted millions of lives across India, Africa, the UK, and the United States by delivering high-quality eye care in underserved regions. The foundation remains committed to its mission of creating a world where no child suffers from preventable blindness.
Join the Movement
Dr. Raju passionately called on individuals and organizations to join this noble mission. “Together, let us illuminate young lives and create a world without childhood blindness. Your support can change lives, restore vision, and empower futures,” he urged. “Now, let’s all be part of something extraordinary.”
For those interested in contributing to this remarkable initiative, more information is available at [www.eyefoundationofamerica.







 The Indo American Cultural Association of Edison, under the capable leadership of Nitin Vyas and in partnership with the Consulate of India in New York, held a vibrant International Yoga Day event on June 14 at the Sheraton Hotel in Edison, New Jersey. Despite facing heavy rainfall, the gathering saw an impressive turnout of over 300 yoga enthusiasts, supported by a number of major Indo American organizations. The participants experienced inspiring yoga sessions led by several distinguished instructors.
The Indo American Cultural Association of Edison, under the capable leadership of Nitin Vyas and in partnership with the Consulate of India in New York, held a vibrant International Yoga Day event on June 14 at the Sheraton Hotel in Edison, New Jersey. Despite facing heavy rainfall, the gathering saw an impressive turnout of over 300 yoga enthusiasts, supported by a number of major Indo American organizations. The participants experienced inspiring yoga sessions led by several distinguished instructors. bringing a unique perspective and specialization to the celebration. Among the speakers and instructors was Guru Dileepji, who delivered an inspiring talk that encouraged attendees to embrace the spiritual side of yoga. Mark Becker contributed an insightful discussion that delved into the philosophical roots and benefits of yoga in daily life.
bringing a unique perspective and specialization to the celebration. Among the speakers and instructors was Guru Dileepji, who delivered an inspiring talk that encouraged attendees to embrace the spiritual side of yoga. Mark Becker contributed an insightful discussion that delved into the philosophical roots and benefits of yoga in daily life. Adding to the wholesome theme of the day was a nutritious vegan lunch that was served to all participants. VIP attendees were additionally treated to a special breakfast, emphasizing the event’s broader commitment to health and wellness in every aspect. The carefully curated meals mirrored the yogic philosophy of balance and nourishment.
Adding to the wholesome theme of the day was a nutritious vegan lunch that was served to all participants. VIP attendees were additionally treated to a special breakfast, emphasizing the event’s broader commitment to health and wellness in every aspect. The carefully curated meals mirrored the yogic philosophy of balance and nourishment. fostering unity and harmony within the community. As noted in the closing remarks, the gathering once again demonstrated how yoga serves as a bridge between cultures and beliefs. “This celebration once again showcased yoga’s ability to transcend cultural differences, fostering peace and unity,” remarked a representative of the Indo American Cultural Association.
fostering unity and harmony within the community. As noted in the closing remarks, the gathering once again demonstrated how yoga serves as a bridge between cultures and beliefs. “This celebration once again showcased yoga’s ability to transcend cultural differences, fostering peace and unity,” remarked a representative of the Indo American Cultural Association.
 The morning began with a warm welcome and opening remarks delivered by the event coordinator, Nitin Vyas, who set the tone for the day’s spiritual and health-focused activities. The official launch of the event was marked by a ceremonial lighting of the lamp led by Deputy Consulate General Vishal Harsh. In his inaugural address, Harsh stressed yoga’s significance in promoting balanced well-being and a healthy lifestyle, highlighting its growing global influence. “Yoga offers a holistic path to health and well-being,” he stated, drawing attention to the practice’s enduring relevance in modern life.
The morning began with a warm welcome and opening remarks delivered by the event coordinator, Nitin Vyas, who set the tone for the day’s spiritual and health-focused activities. The official launch of the event was marked by a ceremonial lighting of the lamp led by Deputy Consulate General Vishal Harsh. In his inaugural address, Harsh stressed yoga’s significance in promoting balanced well-being and a healthy lifestyle, highlighting its growing global influence. “Yoga offers a holistic path to health and well-being,” he stated, drawing attention to the practice’s enduring relevance in modern life. support mobility and joint health. Geeta Ji, from RadiantRays Yoga, offered a physically engaging session tailored for strength and flexibility enhancement.
support mobility and joint health. Geeta Ji, from RadiantRays Yoga, offered a physically engaging session tailored for strength and flexibility enhancement.
 Hosted by Eric Adams in partnership with Dr. Raj Bhayani, president of the Federation of Indian Physicians Association, the event was attended by over 150 prominent community, business, and healthcare leaders from across the New York tri-state region, representing Indian, Bangladeshi, Afghanistan, Jewish, Spanish, as well as Americans and Caribbean communities.
Hosted by Eric Adams in partnership with Dr. Raj Bhayani, president of the Federation of Indian Physicians Association, the event was attended by over 150 prominent community, business, and healthcare leaders from across the New York tri-state region, representing Indian, Bangladeshi, Afghanistan, Jewish, Spanish, as well as Americans and Caribbean communities. healthcare professionals. “You continue to do your job. Nothing can signify that more than COVID, when I’ve witnessed the number of healthcare professionals who were in our hospitals, our healthcare centers, who were doing the testing, who were carrying out all the functions, and still had to worry about not infecting their family members at home. They still got up every day and did their job.”
healthcare professionals. “You continue to do your job. Nothing can signify that more than COVID, when I’ve witnessed the number of healthcare professionals who were in our hospitals, our healthcare centers, who were doing the testing, who were carrying out all the functions, and still had to worry about not infecting their family members at home. They still got up every day and did their job.” Other prominent leaders who were honored at the ceremony included; Chintu Patel, founder and CEO of Amneal Pharmaceutical; Al Mason Fintech, entrepreneur; Dr. Shamim Sharma, eminent Cardiologist; Dr. Deepak Nandi, Neuropsychiatrist and entrepreneur; Dr. Atul Kukar, renowned Cardiologist; Gary Schlesinger, Healthcare Community Leader; Ronald Blount Jr, Bronx County Executive; Gary Sikka, President, American Punjab Society; Kanan Patel, founder and CEO of Kayura pharma health and beauty products; Bhavik Patel, Healthcare executive; Ahmad Masoud, IRCM founder; Jabur Chowdhury, young healthcare entrepreneur; and Dr Eyad Hijazin, a prominent physician from the region.
Other prominent leaders who were honored at the ceremony included; Chintu Patel, founder and CEO of Amneal Pharmaceutical; Al Mason Fintech, entrepreneur; Dr. Shamim Sharma, eminent Cardiologist; Dr. Deepak Nandi, Neuropsychiatrist and entrepreneur; Dr. Atul Kukar, renowned Cardiologist; Gary Schlesinger, Healthcare Community Leader; Ronald Blount Jr, Bronx County Executive; Gary Sikka, President, American Punjab Society; Kanan Patel, founder and CEO of Kayura pharma health and beauty products; Bhavik Patel, Healthcare executive; Ahmad Masoud, IRCM founder; Jabur Chowdhury, young healthcare entrepreneur; and Dr Eyad Hijazin, a prominent physician from the region.


 The International Day of Yoga is a day of recognition for yoga, celebrated annually around the world on 21 June, following its adoption by the
The International Day of Yoga is a day of recognition for yoga, celebrated annually around the world on 21 June, following its adoption by the 










 Dr. Kathula along with other AAPI leaders presented before the lawmakers, key issues that affect the delivery of healthcare in the issues in the US. “Fixing Medicare reimbursement cuts, reforming prior authorization processes, addressing scope of practice concerns, fast-tracking green cards for H-1B visa holders, securing equitable Telemedicine payments, and proposing amendments to the Stark Law” were some of the issues AAPI highlighted in their meetings with the lawmakers.
Dr. Kathula along with other AAPI leaders presented before the lawmakers, key issues that affect the delivery of healthcare in the issues in the US. “Fixing Medicare reimbursement cuts, reforming prior authorization processes, addressing scope of practice concerns, fast-tracking green cards for H-1B visa holders, securing equitable Telemedicine payments, and proposing amendments to the Stark Law” were some of the issues AAPI highlighted in their meetings with the lawmakers. encouraged by the momentum. AAPI’s advocacy on these critical topics will remain ongoing,” Dr. Vidya Kora, Co-Chair of AAPI Legislative Affairs Committee.
encouraged by the momentum. AAPI’s advocacy on these critical topics will remain ongoing,” Dr. Vidya Kora, Co-Chair of AAPI Legislative Affairs Committee.

 “AAPI Legislative Day is a flagship annual event that is eagerly awaited to rekindle and renew our energy in bringing up the issues that we need to bring to the attention of national policy makers and leaders of the US Congress on Capitol Hill,” said Dr. Amit Chakrabarty, president-elect of AAPI. “It is a tradition of nearly three decades, which has brought many important transformations in National Healthcare policies that have helped Physicians of Indian Origin. Now, it is the need of the day to renew our friendship with new leadership under President Donald Trump and Vice President J D Vance and brief the Congressional leadership on issues that are important to us.”
“AAPI Legislative Day is a flagship annual event that is eagerly awaited to rekindle and renew our energy in bringing up the issues that we need to bring to the attention of national policy makers and leaders of the US Congress on Capitol Hill,” said Dr. Amit Chakrabarty, president-elect of AAPI. “It is a tradition of nearly three decades, which has brought many important transformations in National Healthcare policies that have helped Physicians of Indian Origin. Now, it is the need of the day to renew our friendship with new leadership under President Donald Trump and Vice President J D Vance and brief the Congressional leadership on issues that are important to us.”
 The ceremony concluded with a symbolic lamp-lighting, signifying hope and new beginnings for children with CVI. Attendees were deeply moved by a special cultural performance by children with disabilities, demonstrating their incredible resilience and talent.
The ceremony concluded with a symbolic lamp-lighting, signifying hope and new beginnings for children with CVI. Attendees were deeply moved by a special cultural performance by children with disabilities, demonstrating their incredible resilience and talent.
















































 Sam shared his life story with the audience during a Fund Raiser organized by
Sam shared his life story with the audience during a Fund Raiser organized by  training 500 healthcare professionals in
training 500 healthcare professionals in  Lord Rami Ranger, a well-known philanthropist, and successful businessman from the United Kingdom, while echoing the mission of EFA said, “Childhood blindness is a solvable problem, but it requires our collective action.” According to
Lord Rami Ranger, a well-known philanthropist, and successful businessman from the United Kingdom, while echoing the mission of EFA said, “Childhood blindness is a solvable problem, but it requires our collective action.” According to 

 Deliver life-saving Retinopathy of Prematurity screenings and treatments to premature infants.
Deliver life-saving Retinopathy of Prematurity screenings and treatments to premature infants.
 Organized by a team of young Medical Students and Residents of Indian origin, the Medical Scholars Summit was planned and organized by an MSRF Executive Board, led by Priya Uppal, President of MSRF; Priyanka Kolli, President-Elect; Sohi Mistry, Vice President; Priyal Shah, Treasurer; and Drishti Patel, Secretary of MSRF.
Organized by a team of young Medical Students and Residents of Indian origin, the Medical Scholars Summit was planned and organized by an MSRF Executive Board, led by Priya Uppal, President of MSRF; Priyanka Kolli, President-Elect; Sohi Mistry, Vice President; Priyal Shah, Treasurer; and Drishti Patel, Secretary of MSRF. event, with highlights that included our residency and fellowship panel – where attendees had the opportunity to ask questions directly of these program directors from a variety of surgical and non-surgical specialties, our medical school admissions Q&A from the Dean of Warren Alpert Medical School of Brown University, and an MCAT advice lecture from a 520+ scorer.”
event, with highlights that included our residency and fellowship panel – where attendees had the opportunity to ask questions directly of these program directors from a variety of surgical and non-surgical specialties, our medical school admissions Q&A from the Dean of Warren Alpert Medical School of Brown University, and an MCAT advice lecture from a 520+ scorer.” “The 2-day-long Summit was packed with academic sessions that were interactive, with participants having an opportunity to actively engage in discussions and enhance their knowledge on a wide range of topics relevant to Medical Students and Residents, who seek guidance on ways to pursue their careers most effectively,” said Dr. Sunil Kaza, Chair of APPI BOT.
“The 2-day-long Summit was packed with academic sessions that were interactive, with participants having an opportunity to actively engage in discussions and enhance their knowledge on a wide range of topics relevant to Medical Students and Residents, who seek guidance on ways to pursue their careers most effectively,” said Dr. Sunil Kaza, Chair of APPI BOT. Modi offered insights on Financial Wellness. Samir Pancholy, MD led a session on Service Project Pursuing Graduate Medical Education. Global Medicine and India: Lessons, Opportunities, and Challenges for the Next Generation of Physicians was presented by Dr. Kumar Belani, MD.
Modi offered insights on Financial Wellness. Samir Pancholy, MD led a session on Service Project Pursuing Graduate Medical Education. Global Medicine and India: Lessons, Opportunities, and Challenges for the Next Generation of Physicians was presented by Dr. Kumar Belani, MD. Dr. Raj Bhayani, Secretary of AAPI pointed out that, “In addition to several programs in the United States and in India, AAPI has been in the forefront, advocating for the interests of the medical fraternity and organizing regular CME programs, health & wellness events, and financial workshops for its members and outreach, public health education, and advocacy activities for the community both locally and internationally.”
Dr. Raj Bhayani, Secretary of AAPI pointed out that, “In addition to several programs in the United States and in India, AAPI has been in the forefront, advocating for the interests of the medical fraternity and organizing regular CME programs, health & wellness events, and financial workshops for its members and outreach, public health education, and advocacy activities for the community both locally and internationally.”






 The program was designed and directed by Dr.Vemuri S Murthy, a renowned Indo-US Resuscitation Medicine expert from the Department of Emergency Medicine, University of Illinois College of Medicine, Chicago, Illinois, and an alumnus of Guntur Medical College.
The program was designed and directed by Dr.Vemuri S Murthy, a renowned Indo-US Resuscitation Medicine expert from the Department of Emergency Medicine, University of Illinois College of Medicine, Chicago, Illinois, and an alumnus of Guntur Medical College. for international collaborations in the healthcare sector to enhance outcomes of Heart Emergencies and Sudden Cardiac Arrests which are more prevalent among Indians and the Indian Diaspora.
for international collaborations in the healthcare sector to enhance outcomes of Heart Emergencies and Sudden Cardiac Arrests which are more prevalent among Indians and the Indian Diaspora.
 In this context, The American Association of Physicians of Indian Origin (AAPI), in collaboration with Heartfulness Meditation and the American Heart Association, embarked on a mission to educate and train its members and provide opportunities to promote self-care, improve physician wellness, and reduce burnout, with focus on lifestyle modifications in the treatment of chronic diseases, including cancer, at Kanha Shanti Vanam in Hyderabad, Telangana, India on
In this context, The American Association of Physicians of Indian Origin (AAPI), in collaboration with Heartfulness Meditation and the American Heart Association, embarked on a mission to educate and train its members and provide opportunities to promote self-care, improve physician wellness, and reduce burnout, with focus on lifestyle modifications in the treatment of chronic diseases, including cancer, at Kanha Shanti Vanam in Hyderabad, Telangana, India on 
 The MSRF & PreMed Medical Scholars Summit is led by an Executive Board comprising of Manan Pancholy, President; Rohan Chopra, Vice President; Prerak Shah, Secretary; Arjun Gangasani, Treasurer.
The MSRF & PreMed Medical Scholars Summit is led by an Executive Board comprising of Manan Pancholy, President; Rohan Chopra, Vice President; Prerak Shah, Secretary; Arjun Gangasani, Treasurer. Niraj Kothari, MD will present his insightful session on Pioneering Advanced Practices in Medicine, while Deepen Modi will offer insights on Financial Wellness. Samir Pancholy, MD will lead a session on Service Project Pursuing Graduate Medical Education. Global Medicine and India: Lessons, Opportunities, and Challenges for the Next Generation of Physicians will be presented by Dr. Kumar Belani, MD.
Niraj Kothari, MD will present his insightful session on Pioneering Advanced Practices in Medicine, while Deepen Modi will offer insights on Financial Wellness. Samir Pancholy, MD will lead a session on Service Project Pursuing Graduate Medical Education. Global Medicine and India: Lessons, Opportunities, and Challenges for the Next Generation of Physicians will be presented by Dr. Kumar Belani, MD. Dr. Raj Bhayani, Secretary of AAPI pointed out that, “In addition to several programs in the United States and in India, AAPI has been in the forefront, advocating for the interests of the medical fraternity and organizing regular CME programs, health & wellness events, and financial workshops for its members and outreach, public health education, and advocacy activities for the community both locally and internationally.”
Dr. Raj Bhayani, Secretary of AAPI pointed out that, “In addition to several programs in the United States and in India, AAPI has been in the forefront, advocating for the interests of the medical fraternity and organizing regular CME programs, health & wellness events, and financial workshops for its members and outreach, public health education, and advocacy activities for the community both locally and internationally.”
 Pointing to studies, Dr. Kathula said that almost one in three in this group may die from heart disease before 65 years of age. In India, heart disease remains the number one cause of death. Common risk factors are smoking and a diet high in sugar, salt, refined grains, and fat. A large number of South Asians appear to have “insulin resistance”, a condition in which the body does not utilize insulin efficiently, resulting in Diabetes, which leads to a significant number of heart-related problems. Lack of adequate exercise, stress, and genetic predisposition are also contributing factors.
Pointing to studies, Dr. Kathula said that almost one in three in this group may die from heart disease before 65 years of age. In India, heart disease remains the number one cause of death. Common risk factors are smoking and a diet high in sugar, salt, refined grains, and fat. A large number of South Asians appear to have “insulin resistance”, a condition in which the body does not utilize insulin efficiently, resulting in Diabetes, which leads to a significant number of heart-related problems. Lack of adequate exercise, stress, and genetic predisposition are also contributing factors. The Honorable Consul General of the U.S. in Hyderabad, Jennifer Larson, was the chief guest and spoke highly of the contributions of Indian physicians in the U.S. and their vital role in the American healthcare system. Dr. Nageshwar Reddy, chief of AIG, addressed the audience, praising AAPI’s efforts.
The Honorable Consul General of the U.S. in Hyderabad, Jennifer Larson, was the chief guest and spoke highly of the contributions of Indian physicians in the U.S. and their vital role in the American healthcare system. Dr. Nageshwar Reddy, chief of AIG, addressed the audience, praising AAPI’s efforts.



 Surveys have shown MD burnout of 38% in 2020 which increased to 61% in 2021 caused many physicians to leave practice or cut back on hours. The Covid pandemic certainly contributed to the peak of this phenomenon. some of the fundamental sources of burnout for physicians existed before the pandemic, and they persist after.
Surveys have shown MD burnout of 38% in 2020 which increased to 61% in 2021 caused many physicians to leave practice or cut back on hours. The Covid pandemic certainly contributed to the peak of this phenomenon. some of the fundamental sources of burnout for physicians existed before the pandemic, and they persist after. Stressing the importance of registering for the Bone Marro donation, Dr. Suni Kaza, Chair of AAPI BOT said, “You could be a patient’s only match-their only hope for a cure. When you register, you’re committing to donating to any patient in the world. But because a decision not to donate can be life-threatening to the patient, please think seriously about your commitment before joining the registry. And, be aware that there are absolutely no complications to the donor from this donation procedure.”
Stressing the importance of registering for the Bone Marro donation, Dr. Suni Kaza, Chair of AAPI BOT said, “You could be a patient’s only match-their only hope for a cure. When you register, you’re committing to donating to any patient in the world. But because a decision not to donate can be life-threatening to the patient, please think seriously about your commitment before joining the registry. And, be aware that there are absolutely no complications to the donor from this donation procedure.” Among the many initiatives Dr. Raju has undertaken, the upcoming Fundraiser in New Delhi is a pan-India Roll Out Program with the objective of raising $500,000, which will be matched by the Eye Foundation of America. The funds raised will be utilized towards establishing 100 ROP screening centers across India; Training 500 healthcare professionals in ROP screening and treatment; and, Treating 10,000 ROP-affected babies annually across India.
Among the many initiatives Dr. Raju has undertaken, the upcoming Fundraiser in New Delhi is a pan-India Roll Out Program with the objective of raising $500,000, which will be matched by the Eye Foundation of America. The funds raised will be utilized towards establishing 100 ROP screening centers across India; Training 500 healthcare professionals in ROP screening and treatment; and, Treating 10,000 ROP-affected babies annually across India.  For the past four decades, Dr. Raju and the EFA have been actively and tirelessly on a crusade to eliminate avoidable blindness in areas plagued by poverty and poor access to medical care. The EFA’s mission is to eliminate
For the past four decades, Dr. Raju and the EFA have been actively and tirelessly on a crusade to eliminate avoidable blindness in areas plagued by poverty and poor access to medical care. The EFA’s mission is to eliminate  The Goutami Institute has a wing dedicated exclusively for children, and the EFA has future plans to build a service and research eye hospital in India where no child will be denied treatment and children from around the world can come to receive services. Dr. Raju and the EFA are also committed to finding new cures for age-old eye disease in children.
The Goutami Institute has a wing dedicated exclusively for children, and the EFA has future plans to build a service and research eye hospital in India where no child will be denied treatment and children from around the world can come to receive services. Dr. Raju and the EFA are also committed to finding new cures for age-old eye disease in children.  Heart attacks remain a leading cause of death in the United States, with someone experiencing one every forty seconds. Shiny Xavier and Laicy Mecheril, two experienced Nurse Practitioners, conducted an interactive session titled “Myocardial Infarction: Timely Intervention”. They brought up the latest knowledge and evidence-based interventions in treating heart attacks. Bessy Thankavelu, another expert in the field, presented “A Perspective on Women and Heart Disease” and discussed how heart attack symptoms can differ for women, often leading to misdiagnosis and delayed treatment.
Heart attacks remain a leading cause of death in the United States, with someone experiencing one every forty seconds. Shiny Xavier and Laicy Mecheril, two experienced Nurse Practitioners, conducted an interactive session titled “Myocardial Infarction: Timely Intervention”. They brought up the latest knowledge and evidence-based interventions in treating heart attacks. Bessy Thankavelu, another expert in the field, presented “A Perspective on Women and Heart Disease” and discussed how heart attack symptoms can differ for women, often leading to misdiagnosis and delayed treatment. Dr. Kathula was invited by the Hon. Consulate General of India in New York, Mr Binay Pradhan to participate and address the important meeting with distinguished Members of Parliament from India, as well as prominent leaders of the Indian-American community. This meeting offered a unique opportunity for meaningful exchanges on a wide range of topics that are critical to both India and the Indian diaspora in the United States.
Dr. Kathula was invited by the Hon. Consulate General of India in New York, Mr Binay Pradhan to participate and address the important meeting with distinguished Members of Parliament from India, as well as prominent leaders of the Indian-American community. This meeting offered a unique opportunity for meaningful exchanges on a wide range of topics that are critical to both India and the Indian diaspora in the United States. Diaspora members who were part of the meeting included Edison Mayor Sam Joshi , Dr. Samin K. Sharma, Dr. Thomas Abraham, Mr. Gaurav Verma, Prof. Indrajit Saluja, Dr. Avinash Gupta, Mr. Rakesh Kaul, Dr. Hari Shukla, and Mr. Jatinder Singh Bakshi, who shared their perspectives on different aspects of the Indian-American relationship and expressed a strong desire to give back to the motherland.
Diaspora members who were part of the meeting included Edison Mayor Sam Joshi , Dr. Samin K. Sharma, Dr. Thomas Abraham, Mr. Gaurav Verma, Prof. Indrajit Saluja, Dr. Avinash Gupta, Mr. Rakesh Kaul, Dr. Hari Shukla, and Mr. Jatinder Singh Bakshi, who shared their perspectives on different aspects of the Indian-American relationship and expressed a strong desire to give back to the motherland. In addition, he participated in an interview on BBC and with the Press Trust of India, where he addressed critical issues surrounding physician safety in India and the contributions of Indian American physicians.
In addition, he participated in an interview on BBC and with the Press Trust of India, where he addressed critical issues surrounding physician safety in India and the contributions of Indian American physicians. In collaboration with AAPI leadership., Dr. Kathula has been credited with successfully “conducting a fair election for the Vice President of AAPI, ensuring transparency and integrity in our electoral processes. This is crucial for maintaining trust within our organization,: said Dr. Kathula.
In collaboration with AAPI leadership., Dr. Kathula has been credited with successfully “conducting a fair election for the Vice President of AAPI, ensuring transparency and integrity in our electoral processes. This is crucial for maintaining trust within our organization,: said Dr. Kathula. Along with Dr. Kathula, Dr. Amit Chakrabarty serves as the President-Elect of AAPI, Dr. Meher Medavaram, Vice President, Dr. Raj Bhayani, Secretary, and Shirish Patel, Treasurer of AAPI for the year 2024-25. Dr. Sunil Kaza is the Chair of AAPI Board of Trustees. Representing the young physicians of Indian origin, Dr. Shefali Kothary serves as the YPS President and Dr. Oriya Uppal is the MSRF President for the year 2024-25.
Along with Dr. Kathula, Dr. Amit Chakrabarty serves as the President-Elect of AAPI, Dr. Meher Medavaram, Vice President, Dr. Raj Bhayani, Secretary, and Shirish Patel, Treasurer of AAPI for the year 2024-25. Dr. Sunil Kaza is the Chair of AAPI Board of Trustees. Representing the young physicians of Indian origin, Dr. Shefali Kothary serves as the YPS President and Dr. Oriya Uppal is the MSRF President for the year 2024-25.