Global omega-3 deficiency affects 76% of people worldwide, significantly increasing risks for heart disease, cognitive decline, and chronic inflammation, according to a new study.
A recent analysis has revealed that more than three-quarters of the global population is not meeting the recommended intake levels of omega-3 fatty acids, a nutrient gap that could lead to increased risks of heart disease, cognitive decline, chronic inflammation, and vision problems. This finding comes from a study published in *Nutrition Research Reviews*, conducted by researchers from the University of East Anglia, the University of Southampton, and Holland & Barrett.
The review indicates that 76% of individuals worldwide are falling short of the recommended daily intake of two essential omega-3 fats: eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Global health authorities recommend that most adults aim for at least 250 milligrams of EPA and DHA per day, yet actual intake levels are significantly lower in many regions.
To delve deeper into the health implications of low omega-3 intake, Fox News Digital consulted with Michelle Routhenstein, a preventive cardiology dietitian based in New York at Entirely Nourished. Routhenstein confirmed that low omega-3 levels can adversely affect heart health, cognitive function, and inflammation throughout the body.
According to Routhenstein, insufficient omega-3 intake can elevate the risk of heart attacks and sudden cardiac death. It is also associated with higher triglyceride levels, irregular heart rhythms, and plaque buildup in the arteries. Furthermore, inadequate omega-3 levels have been linked to cognitive decline, a heightened risk of Alzheimer’s disease, and increased rates of depression.
Routhenstein pointed out that low omega-3 levels may exacerbate inflammation in autoimmune conditions, such as psoriasis, and can negatively impact eye health, as omega-3s play a crucial structural role in the retina.
To improve omega-3 levels, Routhenstein emphasized the importance of understanding both the required intake and the best sources of these essential fats. She noted that the richest dietary sources of EPA and DHA are oily fish, including salmon, mackerel, sardines, herring, trout, and anchovies. For many individuals, consuming oily fish three to four times per week can be beneficial.
For those who do not regularly eat fish, omega-3 supplements can help raise EPA and DHA levels to healthier ranges. Routhenstein advised that dosing for omega-3 supplements should be tailored based on lab results, medications, omega-3 levels, and overall medical history. Generally, moderate, quality-controlled supplements are considered safe for most individuals.
There is also evidence supporting the use of prescription-strength omega-3 products. Routhenstein noted that high-dose EPA, such as 4 grams per day of icosapent ethyl, has been shown to reduce major cardiovascular events in certain high-risk populations. However, similar doses of mixed EPA/DHA have not consistently demonstrated the same benefits.
Testing omega-3 levels can provide insight into whether an individual’s intake is adequate. The omega-3 index, a blood test that measures EPA and DHA in red blood cells, is regarded as one of the most reliable methods for assessing omega-3 status. Routhenstein explained that levels around 8% are associated with a lower cardiovascular risk, while levels below approximately 4% are considered low.
Understanding one’s baseline omega-3 levels can help guide more personalized dietary and supplementation decisions. Individuals who are uncertain about their omega-3 status or whether supplementation is appropriate are encouraged to consult with a healthcare provider to determine the best course of action.
According to Routhenstein, addressing omega-3 deficiency could play a significant role in improving overall health and reducing the risk of serious health issues.











































 reconnection with India’s timeless healing traditions. “It’s both remarkable and ironic that it took us this long to formally embrace Ayurveda, a tradition nurtured here at The Raj for over 30 years,” noted AAPI President Dr. Amit Chakrabarty. “We’re thrilled to finally bridge this gap and offer our members a handcrafted retreat designed to rejuvenate body, mind, and spirit.”
reconnection with India’s timeless healing traditions. “It’s both remarkable and ironic that it took us this long to formally embrace Ayurveda, a tradition nurtured here at The Raj for over 30 years,” noted AAPI President Dr. Amit Chakrabarty. “We’re thrilled to finally bridge this gap and offer our members a handcrafted retreat designed to rejuvenate body, mind, and spirit.”


















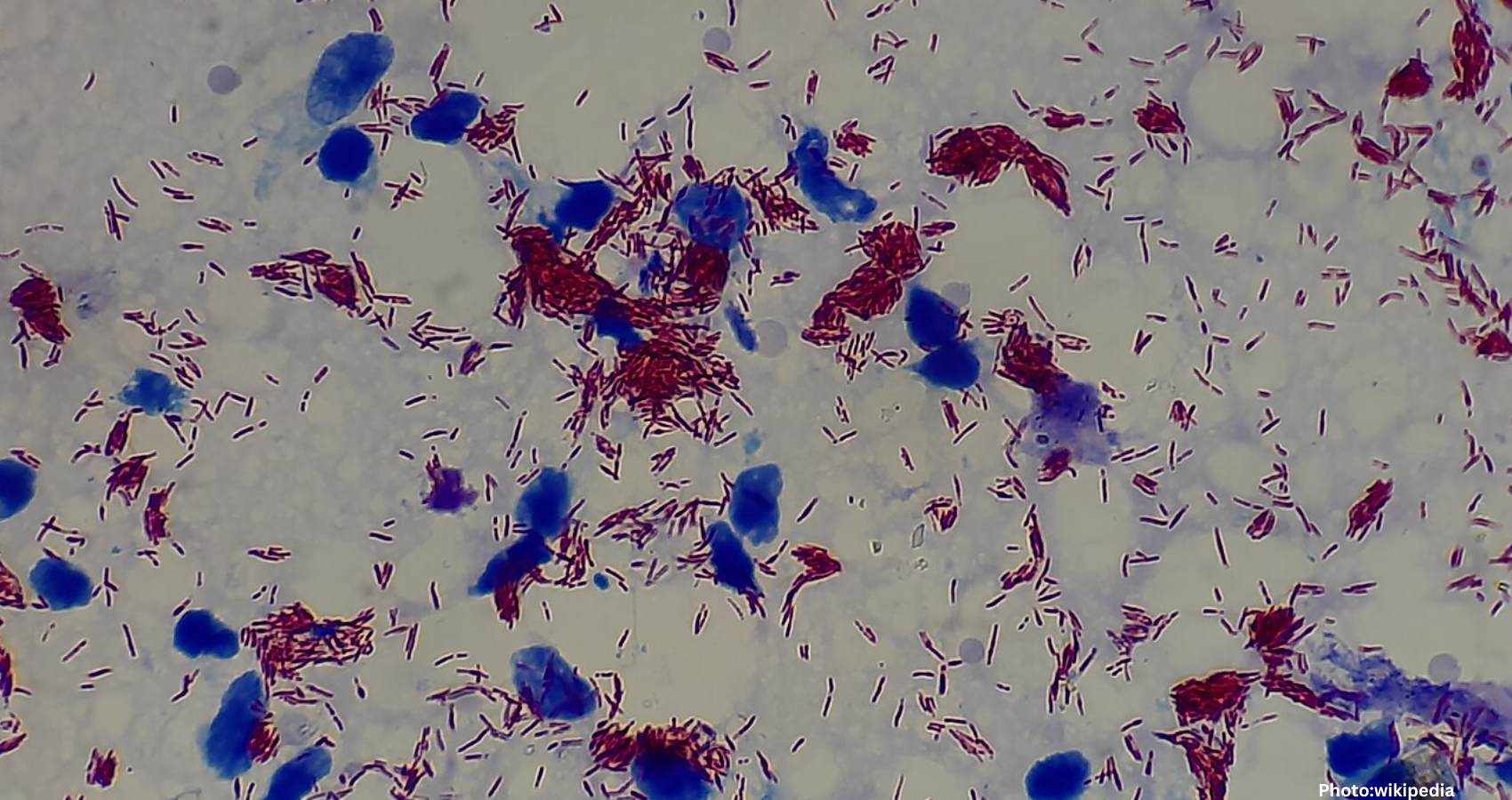
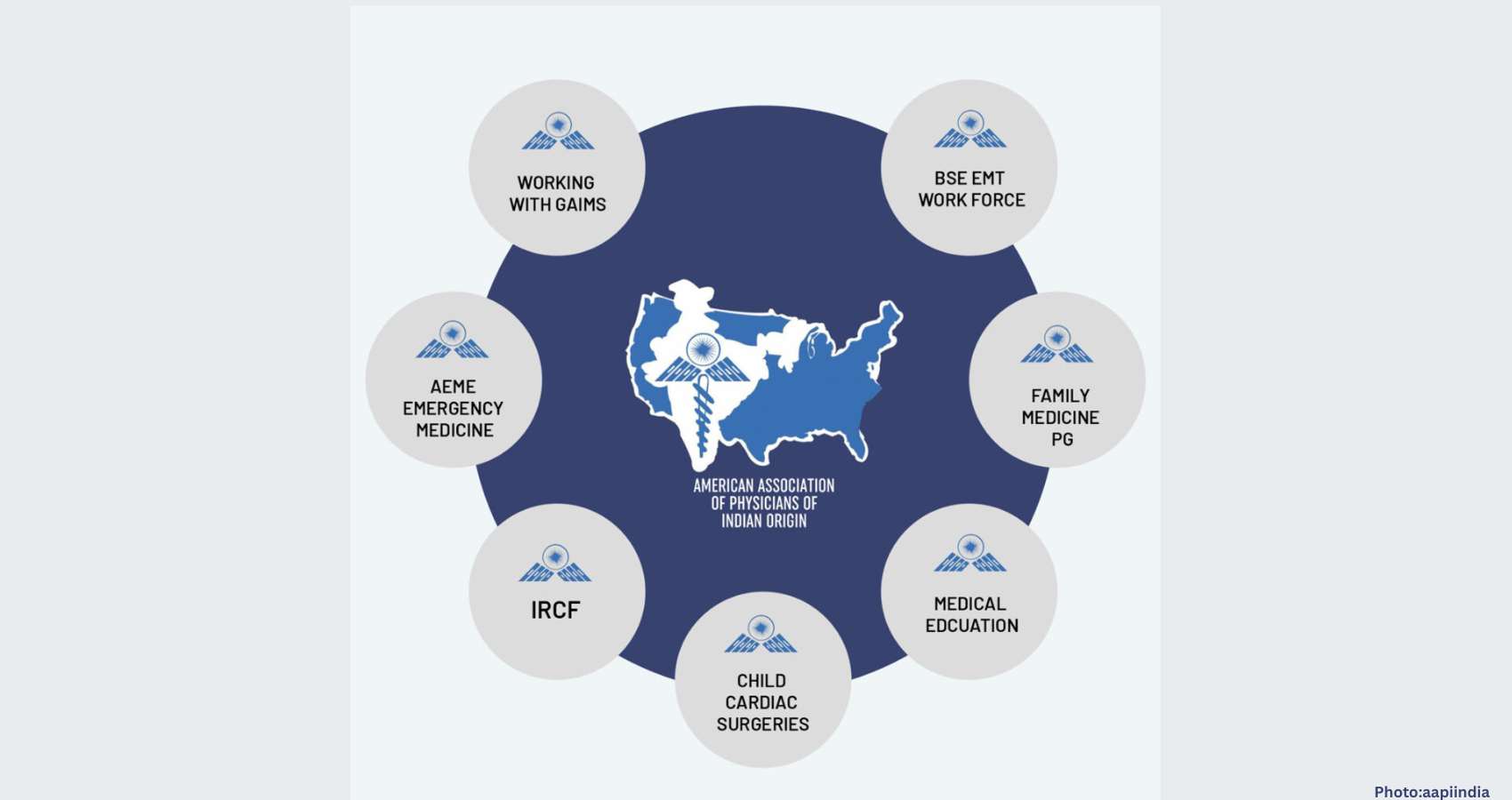
 The American Association of Physicians of Indian Origin (AAPI) is set to host its 19th Annual Global Health Summit (GHS) in Bhubaneswar, Odisha, from January 9 to 11, 2026. This landmark event, drawing hundreds of physicians, researchers, and policymakers from across the globe, will serve as a pivotal forum to address India’s most urgent health challenges: Tuberculosis (TB), Diabetes, the integration of Ayurveda with modern medicine, and the adoption of cutting-edge health technology.
The American Association of Physicians of Indian Origin (AAPI) is set to host its 19th Annual Global Health Summit (GHS) in Bhubaneswar, Odisha, from January 9 to 11, 2026. This landmark event, drawing hundreds of physicians, researchers, and policymakers from across the globe, will serve as a pivotal forum to address India’s most urgent health challenges: Tuberculosis (TB), Diabetes, the integration of Ayurveda with modern medicine, and the adoption of cutting-edge health technology.