Diagnosing and treating prostate cancer has long stirred controversy and ambiguity. One focal point of debate involves prostate-specific antigen (PSA) testing, a blood examination identifying a distinctive protein that may unveil cancer even in asymptomatic patients. Since its inception in the early 1990s, PSA testing garnered widespread acceptance with millions conducted annually in the U.S. Nonetheless, in 2012, a government task force cautioned that this test might lead to overtreating cancers of minimal threat, advocating for a more restrained approach.
While the discourse surrounding PSA testing oscillates, the field has made significant strides in understanding the factors driving rapid growth in certain prostate cancers. These insights have contributed to improved patient prognoses across all disease stages, even in advanced cases. Today, prostate cancer specialists wield an enhanced arsenal of treatment tools and can judiciously assess when intervention is warranted.
The significance of these advancements cannot be overstated, considering prostate cancer remains one of the most prevalent malignancies. Beyond some skin cancers, prostate cancer ranks among the most common cancers affecting men in the U.S. Each year, nearly 270,000 Americans receive a prostate cancer diagnosis, making it the fourth most common cancer globally. Fortunately, most patients diagnosed with prostate cancer can expect to live for many years post-diagnosis, more likely succumbing to unrelated causes.
At its core, prostate cancer manifests as a malignancy within the prostate gland, responsible for producing fluid that mixes with sperm to form semen. Situated in front of the rectum, below the bladder, and above the penis, the prostate cancer spectrum encompasses four major stages.
Initially, localized tumors confine themselves within the prostate gland. Subsequently, a “regionally advanced” variant of the disease remains in close proximity to the prostate. Metastatic prostate cancers extend beyond the gland, spreading to other body parts. The advent of enhanced diagnostic imaging tests has facilitated the characterization of oligometastatic prostate cancer, marking a stage between localized and widely dispersed metastatic disease. Noteworthy discoveries over the past decade have revolutionized the approach to each prostate cancer type, with ongoing advancements anticipated for years to come.
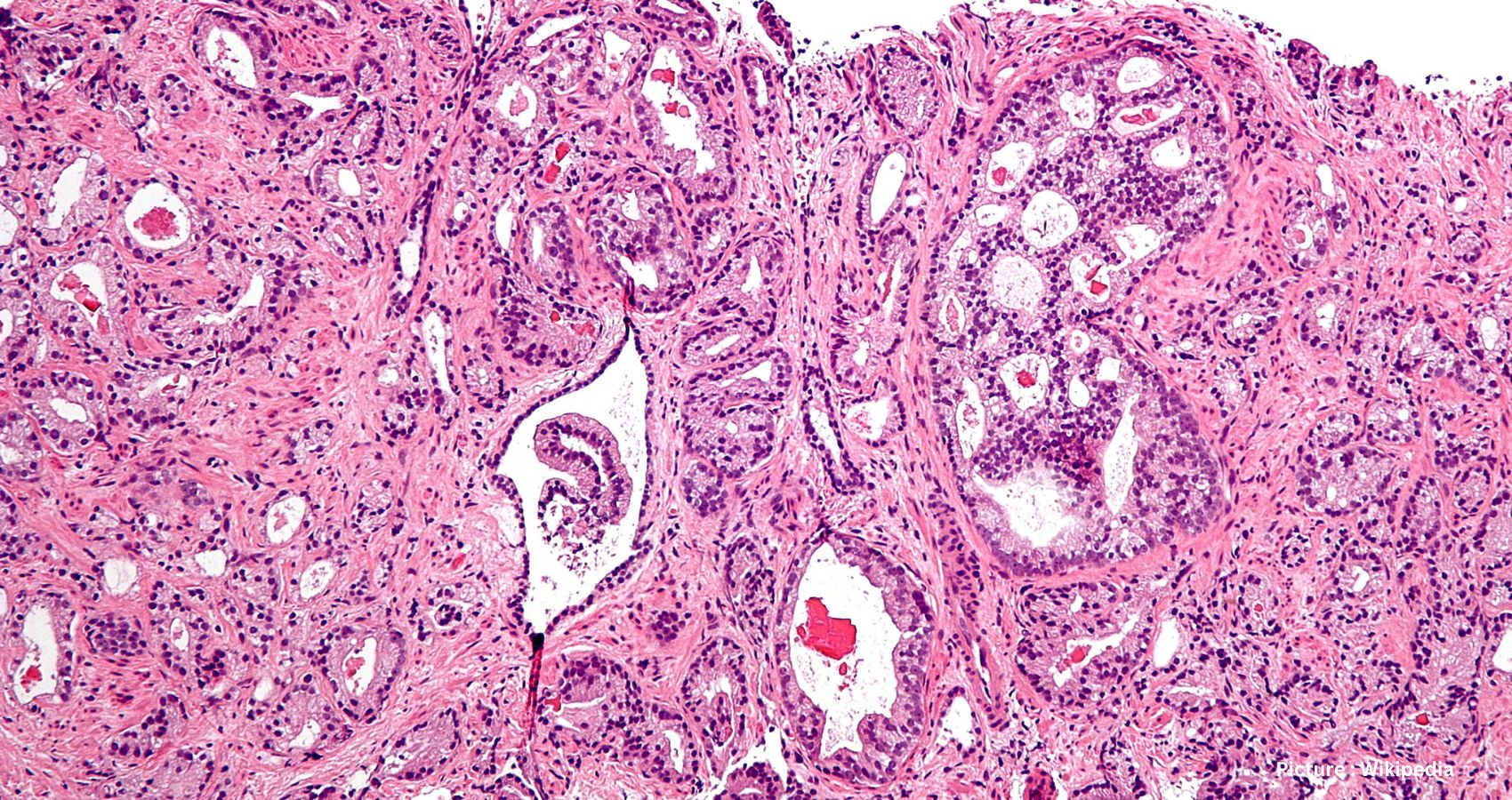
In terms of treatment, the initial steps for individuals with localized cancer involve risk assessment. Physicians gauge the potential for eliminating or curing cancer through local treatments, typically surgery or radiation, and the likelihood of recurrence. This assessment relies on PSA results, physical prostate gland examinations, and tumor cell inspection from biopsies.
The approach to elevated PSA levels in patients continues to evolve. Traditionally, physicians conducted rectal examinations followed by needle biopsies to procure prostate tissue snippets. However, technological advancements now allow for perineal biopsies, conducted outpatient without general anesthesia, mitigating infection risks and antibiotic needs. Notably, MRI scans are increasingly replacing biopsies, aiding in identifying clinically significant cancers while sparing patients unnecessary treatment for clinically insignificant ones.
Following a prostate cancer diagnosis, treatment decisions have historically sparked contentious debates akin to those surrounding diagnosis. Recent research from the U.K. sheds light on this matter, with findings suggesting that “active surveillance,” involving delayed or avoided treatment, is increasingly offered post-diagnosis. Rigorous monitoring, including PSA testing, physical prostate examinations, and urinary symptom assessments, is now common practice, even for patients with more concerning tumors.
For cancers displaying intermediate- or high-risk features, monitoring disease progression entails bone and abdominal-pelvic CT scans, though these may miss small metastatic areas, leading to understaging. Advanced scanning techniques combining PET and CT are addressing this issue, allowing for more precise diagnostic testing.
Such scans, particularly PSMA PET-CT scans, enable the identification of small metastatic deposits, paving the way for metastasis-directed therapy (MDT). MDT targets cancer-containing lymph nodes or bony areas with radiation or surgical removal, yielding promising outcomes, including long-term remission in some cases.
Additionally, advancements in hormone therapy for advanced disease are noteworthy. Traditional androgen deprivation therapy (ADT) mainly targets testosterone produced by the testicles, but newer approaches aim to block androgen production by the adrenal glands or cancer cells, substantially improving survival rates.
Moreover, targeted therapies, such as lutetium-177-PSMA-617, show promise in treating prostate cancer resistant to conventional ADT and chemotherapy. Genetic and genomic testing further enhance treatment efficacy, guiding specific therapies tailored to patients’ mutations for improved outcomes.
These remarkable advances, achieved within a decade, mark a significant stride in prostate cancer oncology. From offering conservative choices for early-stage cancers to managing metastatic diseases with fewer systemic side effects, these innovations are transforming prostate cancer into a manageable chronic condition, prolonging patients’ life expectancy.