An increasing number of states are taking action against Big Tech, the internet, and social media platforms. Montana recently became the first state to entirely ban TikTok, though the enforceability of this new law remains questionable. Other states, such as Arkansas and Utah, have introduced legislation to tighten regulations on social media platforms.
There appear to be three primary objectives behind these legal actions: preventing companies from collecting data on users and their children, safeguarding children online, and striking a balance between users’ rights and responsibilities when posting content online. For instance, should a platform be held accountable if it hosts content that results in harm to someone? As of now, the US Supreme Court has ruled “no.”
As a father of three teenage girls, I find the conversations surrounding smartphones and social media deeply personal. Like many parents, I initially viewed devices as mere entertainment for my children and a means of communication in emergencies. However, my perspective changed after reading Jean Twenge’s book, “iGen: Why Today’s Super-Connected Kids Are Growing Up Less Rebellious, More Tolerant, Less Happy – and Completely Unprepared for Adulthood – and What That Means for the Rest of Us.”
In her book, Twenge, a psychology professor at San Diego State University, argues that Generation Z (or iGen) is experiencing a fundamentally different upbringing than previous generations. She informed me that some of the most significant behavioral changes in human history coincided with the advent of smartphones. According to Twenge, today’s 12th-graders resemble eighth-graders from earlier generations, delaying participation in activities associated with independence and adulthood. They are less likely to socialize, drive, attend prom, or consume alcohol compared to their Gen X counterparts, instead spending more time scrolling through social media feeds. Though they may be physically safer, the long-term impact on their mental and brain health remains uncertain.
Twenge shared with me that she “saw just a very, very sudden change, especially in mental health but also in optimism and expectations … between millennials and iGen or Gen Z.” Her words resonated with me but also alarmed me. As a neurosurgeon, I often rely on evidence to address concerns, but when it comes to new technologies, there is a scarcity of data available. We frequently don’t even know what questions to ask, let alone have answers for them.
Consequently, my wife, Rebecca, and I found ourselves in a challenging and uneasy position: determining the appropriate age, duration, and type of screen time for our three iGen daughters based on limited information. I know I’m not alone in this struggle, as I often hear similar concerns from other parents, viewers, readers, and listeners. This is why my podcast, “Chasing Life,” dedicated an entire season to discussing this topic.
Examining the Data
Obtaining consistent statistics is challenging, but a 2023 survey conducted by reviews.org revealed that approximately 89% of American adults check their phones within 10 minutes of waking up. Astoundingly, the same survey indicated that American adults look at their phones an average of 144 times per day, or once every seven waking minutes!
The numbers for children are even more concerning. A 2022 Pew survey of individuals under 18 years old showed that 46% of American teens reported being online “almost constantly.” Additionally, 35% claimed to be “almost constantly” using one of the top five social media apps: YouTube, TikTok, Instagram, Snapchat, and Facebook.
These statistics may not be surprising, considering the endless content available for consumption. In April 2022, data company Domo reported that over 500 hours of video were uploaded to YouTube every minute on average. Meanwhile, an estimated 1.3 billion photos are shared on Instagram daily, according to a photo industry estimate. Furthermore, Snap Inc. stated that over 4 billion Snaps were sent each day as of 2020.
My daughters, aged 17, 16, and 14, are digital natives who have never experienced life without devices. I often think about how this is not the world they chose, but rather the one we handed to them. My youngest daughter once expressed her wish to be a millennial because that generation had phones without smartphones or social media, so they weren’t constantly tethered to their devices. She says that many teenagers today feel compelled to use social media, fearing they will be left behind otherwise.
Lessons Learned
It’s undeniable that screens and technology play a crucial role in modern life, but managing our interactions with them can be challenging. While working on this season of the podcast, I gained valuable insights from experts in the field.
To summarize my findings, I would highlight three main points:
- Initiate a meaningful conversation with your child, free from distractions and judgment. By discussing their screen usage, social media preferences, and feelings about online interactions, you may gain surprising insights and foster a more open dialogue. Dr. Michael Rich, co-director of the Clinic for Interactive Media and Internet Disorders at Boston Children’s Hospital, emphasizes the importance of understanding the pain points of young patients, saying, “I want to look more at what their life is from the time they wake up to the time they go to sleep.”
- Avoid assuming the worst. While it’s likely that your child spends more time on screens than you’d prefer, not every individual will develop a problem. Dr. Keneisha Sinclair-McBride, a clinical psychologist at Boston Children’s Hospital and an assistant professor of psychology at Harvard Medical School, reminds us that social media isn’t the primary concern for most teens. She explains that the challenges faced by today’s youth are similar to those of previous generations, adding, “It’s not like every kid is going to get mental health treatment because social media is ruining their life. That is definitely not the case at all.”
- Keep in mind the words of author Catherine Price: “Life is what we pay attention to.” This empowering concept reminds us that we have control over our experiences. When using our devices, Price suggests asking ourselves three questions: What for? Why now? What else? She explains, “The point is just to make sure that when we’re using our devices or whatever apps are on our devices, it’s the result of an intentional choice instead of just our minds and our brains being hijacked.”
By following these guidelines and making conscious choices, we can navigate the digital landscape more effectively and maintain a healthy balance in our lives.
Navigating the world of screens While exploring the topic of problematic media use during this podcast season, I’ve considered various metaphors to describe it. Is it an addiction like substances or gambling? Are devices designed to keep us hooked? While there are similarities, one key difference is that it’s not feasible to completely avoid technology.
A more fitting analogy might be food: we need both, but we must be mindful of our consumption. Another comparison could be a car or powerful tool: useful and impressive, but requiring control and proper handling. We should view these small supercomputers as tools, not toys for young children.
Did Rebecca and I flawlessly navigate this with our girls? No, but we didn’t have a precedent. “It didn’t exist when we were young, so we are learning how to manage it ourselves,” Rebecca stated. We’re adapting to the learning curve alongside our children.
The kids will be alright Technology is neither good nor bad; it just is. Gen Z acknowledges this and wants improvements. Advocates like Emma Lembke demand change, and lawmakers and tech executives are starting to listen. Lembke told Congress, “Make no mistake, unregulated social media is a weapon of mass destruction that continues to jeopardize the safety, privacy, and well-being of all American youth. It’s time to act.”
Lembke envisions a future where social media is built differently, with more transparent algorithms, an end to autoplay, and image filters that don’t perpetuate beauty standards. She and her peers are concerned for future generations.
We must learn to make better decisions about our digital diets. Dr. Keneisha Sinclair-McBride reminds us that our time and attention are valuable resources, and we should allocate them wisely.
Starting the screentime conversation Unsure how to discuss internet and social media use with your kids? Here are some conversation prompts:
- Describe your typical phone usage in a day.
- How much time do you spend on your phone daily? Too much, too little, or just right?
- What are your favorite apps, games, or platforms, and why?
- Do you have a healthy relationship with technology and social media? What does that look like?
- Do you have fair screentime boundaries? Are they easy to stick to? Would you change the rules?
- Has technology ever interfered with an activity you wanted to do?
- Do you feel pressure from friends or school to be on your phone?
- Do you know people who misuse technology?
- What concerns you about technology or social media?
- Have you tried reducing screentime? Why, and did it work?
- Are you hopeful for your future? Why or why not?







 In his response to being chosen for the award, Dr. Shivangi said, “I am truly honored to receive this prestigious Xavier University of Aruba award, which has made a worldwide impression as a premier Institute of learning. It’s even a greater honor to be in such distinguished ranks of those present and past honorees, who have made important contributions to healthcare.”
In his response to being chosen for the award, Dr. Shivangi said, “I am truly honored to receive this prestigious Xavier University of Aruba award, which has made a worldwide impression as a premier Institute of learning. It’s even a greater honor to be in such distinguished ranks of those present and past honorees, who have made important contributions to healthcare.”











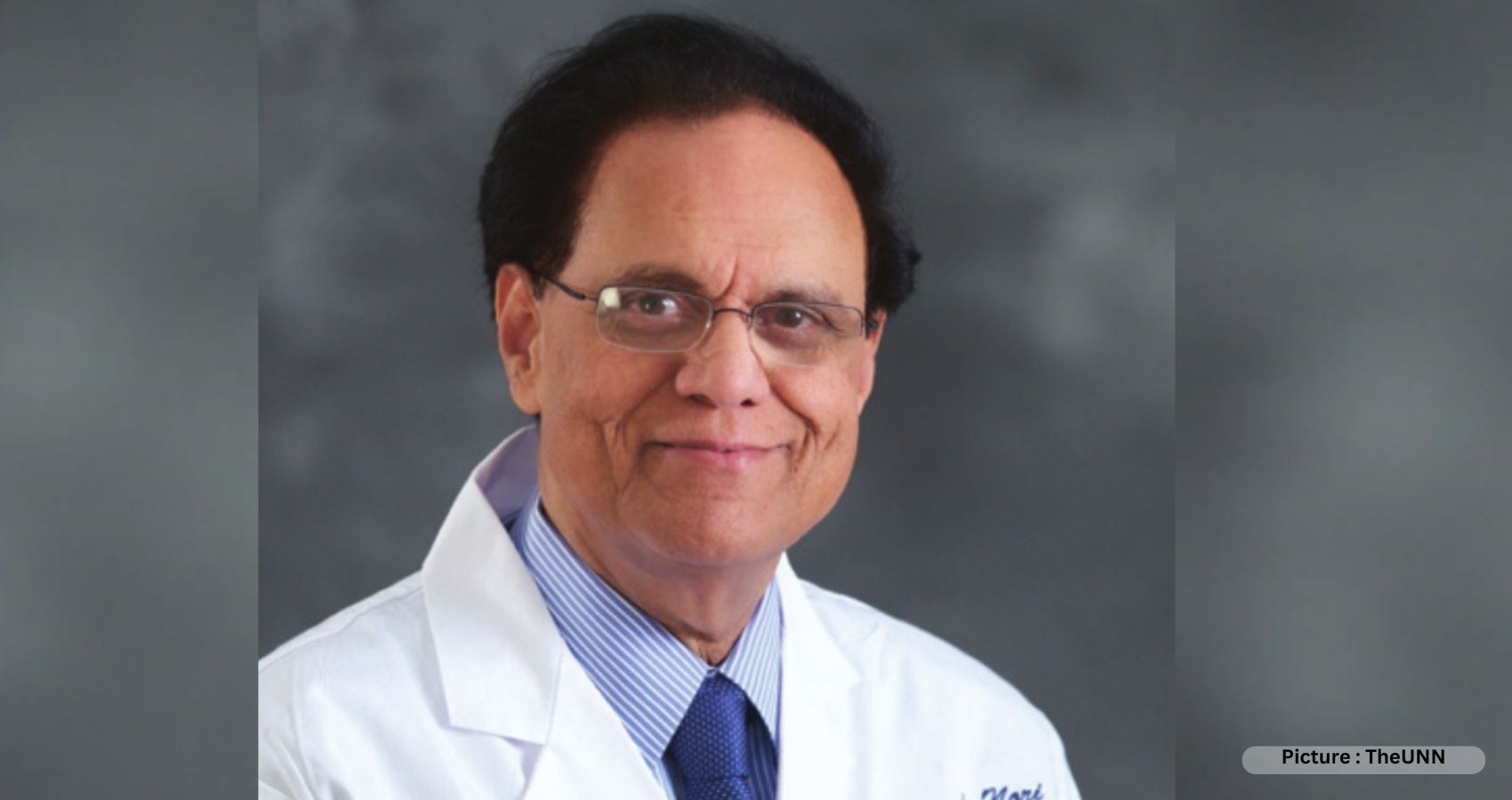

















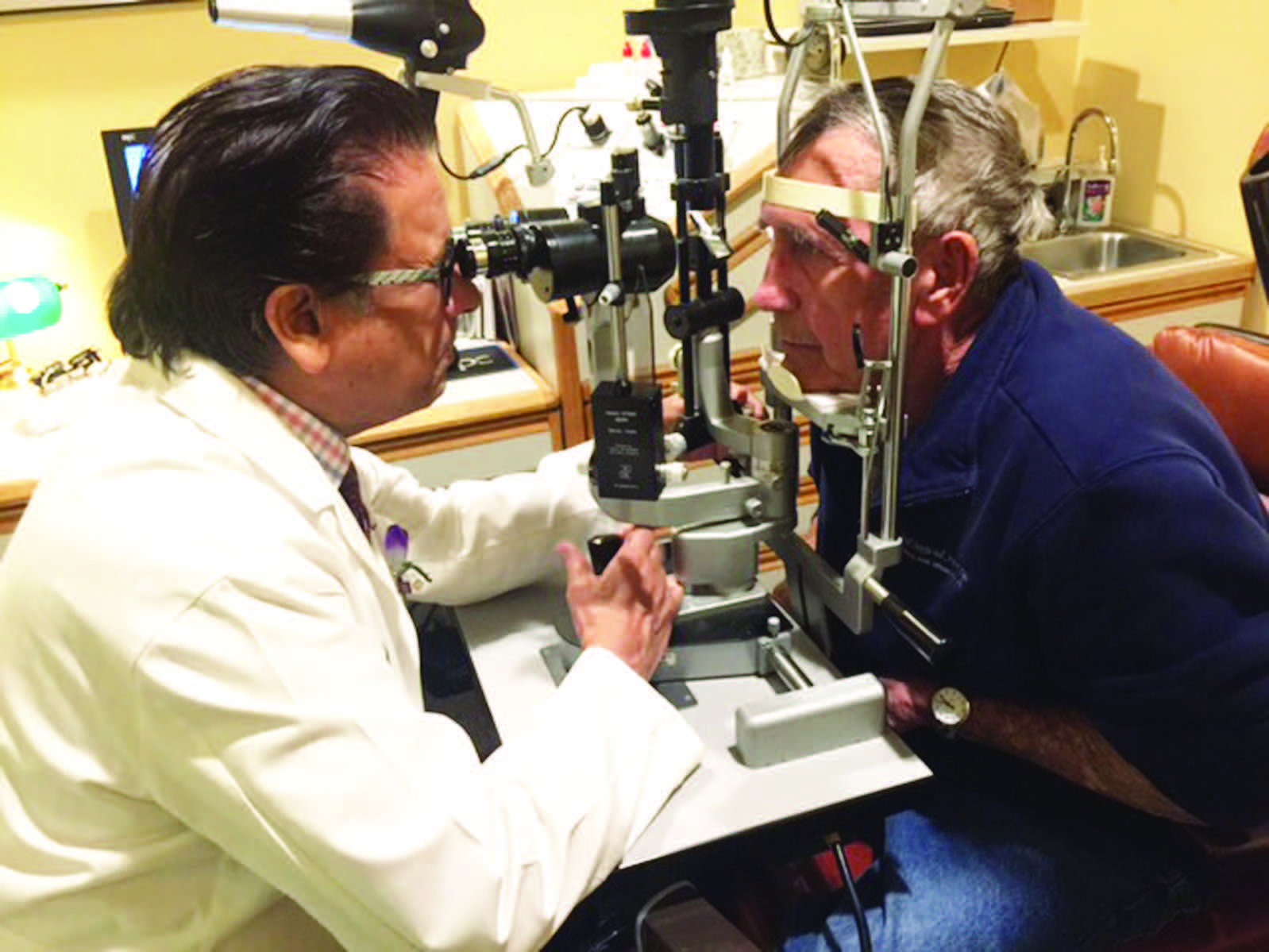 For the past four decades, Dr. Raju and the EFA have been actively and tirelessly on a crusade to eliminate avoidable blindness in areas plagued by poverty and poor access to medical care. The EFA’s mission is to eliminate
For the past four decades, Dr. Raju and the EFA have been actively and tirelessly on a crusade to eliminate avoidable blindness in areas plagued by poverty and poor access to medical care. The EFA’s mission is to eliminate  “I feel so incredibly thankful for my personal and professional gifts, and I make great efforts to share those gifts with those in need of my services,” says Dr. Raju, and he generously gives freely of his own time, money, and medical expertise to help the less fortunate for the past several decades.
“I feel so incredibly thankful for my personal and professional gifts, and I make great efforts to share those gifts with those in need of my services,” says Dr. Raju, and he generously gives freely of his own time, money, and medical expertise to help the less fortunate for the past several decades.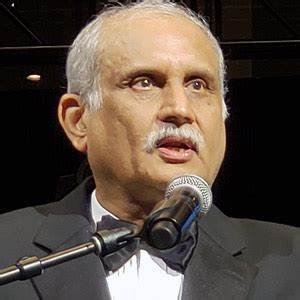 The Institute has provided service to more than 400,000 patients and 50,000 surgeries have been performed. It has become an autonomous institution, and Raju has raised over $6 million to establish and fund the two facilities. “You can never be tired of giving back,” he says. “But to have real success, your intentions should be pure. It is a spiritual act.”
The Institute has provided service to more than 400,000 patients and 50,000 surgeries have been performed. It has become an autonomous institution, and Raju has raised over $6 million to establish and fund the two facilities. “You can never be tired of giving back,” he says. “But to have real success, your intentions should be pure. It is a spiritual act.” Dr. Raju hopes that the AAPI joining and collaborating with successful projects such as the Eye Foundation of America’s children’s project will provide continuity of care and the mission of AAPI will be realized, benefitting millions who need eyecare.
Dr. Raju hopes that the AAPI joining and collaborating with successful projects such as the Eye Foundation of America’s children’s project will provide continuity of care and the mission of AAPI will be realized, benefitting millions who need eyecare.














 During his address, Mr. Patnaik applauded the role played by the various organizations involved with the initiative of saving precious lives. Mr. Krishna Kishore Jasthi, Principal Director of Income Tax (Investigation), Odisha, who is the chief coordinator of the project, welcomed the participants, and explained the objectives of the ground-breaking project, “Saving Lives with Bystander CPR” in Odisha.
During his address, Mr. Patnaik applauded the role played by the various organizations involved with the initiative of saving precious lives. Mr. Krishna Kishore Jasthi, Principal Director of Income Tax (Investigation), Odisha, who is the chief coordinator of the project, welcomed the participants, and explained the objectives of the ground-breaking project, “Saving Lives with Bystander CPR” in Odisha. The participants were given a brief presentation of “Heart Disease Among Women” as part of the program by Dr. Pavitra Kotini-Shah, Assistant Professor in the Department of Emergency Medicine, University of Illinois College of Medicine, Chicago, Illinois, USA. Indo-US Faculty team was honored at the conclusion of the program.
The participants were given a brief presentation of “Heart Disease Among Women” as part of the program by Dr. Pavitra Kotini-Shah, Assistant Professor in the Department of Emergency Medicine, University of Illinois College of Medicine, Chicago, Illinois, USA. Indo-US Faculty team was honored at the conclusion of the program.
 A close friend to the Bush family, he was instrumental in lobbying for the first Diwali celebration in the White House and for President George W. Bush to make his trip to India. He had accompanied President Bill Clinton during his historic visit to India.
A close friend to the Bush family, he was instrumental in lobbying for the first Diwali celebration in the White House and for President George W. Bush to make his trip to India. He had accompanied President Bill Clinton during his historic visit to India.



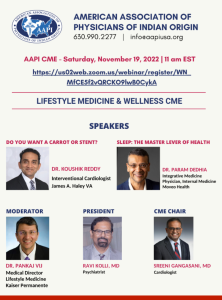
 “The essence of AAPI is educational,” Dr. Kolli added. “That translates into numerous Continuing Medical Education (CME) and non-CME seminars by experts in their fields. The GHS 2023 with the theme of “True and Total Health is the Wellbeing of Mind, Body, and Spirit” has had several CME sessions that focused on Mental Health, Infant and Maternal Mortality as well as various other medical specialty updates, research, and Medical Jeopardy.”
“The essence of AAPI is educational,” Dr. Kolli added. “That translates into numerous Continuing Medical Education (CME) and non-CME seminars by experts in their fields. The GHS 2023 with the theme of “True and Total Health is the Wellbeing of Mind, Body, and Spirit” has had several CME sessions that focused on Mental Health, Infant and Maternal Mortality as well as various other medical specialty updates, research, and Medical Jeopardy.” The second part of the morning session was on Diabetes and Kidney Disease. The scientific presentation on Diabetes Management Update was given by Dr. G.R. Sridhar, while “Diabetic Nephropathy: Current Concepts in Diagnosis” was offered by Dr. Sharma Prabhakar. Dr. K. L. Gupta educated the audience on Lupus Nephritis. “CKD of Unknown Origin & Uddanam Nephropathy” was the theme addressed by Dr. T. Ravi Raju, while “New Insights into the Biology and Mechanism of Renal Fibrosis” was the topic addressed by Dr. Raghu Kalluri. The sessions were moderated by Dr. KAV Subrahmanyam, Dr. K. Dilip Kumar, and Dr. R. K. Sharma.
The second part of the morning session was on Diabetes and Kidney Disease. The scientific presentation on Diabetes Management Update was given by Dr. G.R. Sridhar, while “Diabetic Nephropathy: Current Concepts in Diagnosis” was offered by Dr. Sharma Prabhakar. Dr. K. L. Gupta educated the audience on Lupus Nephritis. “CKD of Unknown Origin & Uddanam Nephropathy” was the theme addressed by Dr. T. Ravi Raju, while “New Insights into the Biology and Mechanism of Renal Fibrosis” was the topic addressed by Dr. Raghu Kalluri. The sessions were moderated by Dr. KAV Subrahmanyam, Dr. K. Dilip Kumar, and Dr. R. K. Sharma. N K Panigrahi opened the session with a brilliant talk on Heart Disease Epidemic, which was followed by an informative session on Heart Failure- What’s New for 2022, presented by Dr. Sreeni Gangasani. Dr. A. Sharath Reddy spoke on Interventional Cardiology Update, and Dr. Brahma Sharma educated the delegates on Current Concepts in Prediction and Prevention of Heart Attacks in South Asians. Structural Heart Disease was the theme of the presentation by Dr. Prasad Chalasani, while Update on Cardiac Surgery was presented by Dr. M. Gopichand.
N K Panigrahi opened the session with a brilliant talk on Heart Disease Epidemic, which was followed by an informative session on Heart Failure- What’s New for 2022, presented by Dr. Sreeni Gangasani. Dr. A. Sharath Reddy spoke on Interventional Cardiology Update, and Dr. Brahma Sharma educated the delegates on Current Concepts in Prediction and Prevention of Heart Attacks in South Asians. Structural Heart Disease was the theme of the presentation by Dr. Prasad Chalasani, while Update on Cardiac Surgery was presented by Dr. M. Gopichand. NATCO Pharma Oncology Session on Sunday, January 8th was chaired by Dr. Satheesh Kathula, Vice President of AAPI, and moderated by Dr. Muralikrishna Voonna and Dr. Sushil Jain. “A focus on newer treatment modalities in Radiation Oncology” was the topic addressed by Dr. Umesh Mahantshetty, while Dr. T. Subramanyeswar Rao spoke about “What’s new in surgical oncology?” An Update on Systemic Therapies for Cancer was provided by Dr. Raghunadharao Digumarti. “Evolving Biology and New Therapies – Strategies to Control Cancer” was the topic addressed by Dr. Raghu Kalluri. An insightful session on Pharmaco economics of cancer drugs – can we afford it?” was presented by Dr. Satheesh Kathula. “India’s unique value proposition towards Medical Tourism” was addressed by Mr. Shaaz Mehmood.
NATCO Pharma Oncology Session on Sunday, January 8th was chaired by Dr. Satheesh Kathula, Vice President of AAPI, and moderated by Dr. Muralikrishna Voonna and Dr. Sushil Jain. “A focus on newer treatment modalities in Radiation Oncology” was the topic addressed by Dr. Umesh Mahantshetty, while Dr. T. Subramanyeswar Rao spoke about “What’s new in surgical oncology?” An Update on Systemic Therapies for Cancer was provided by Dr. Raghunadharao Digumarti. “Evolving Biology and New Therapies – Strategies to Control Cancer” was the topic addressed by Dr. Raghu Kalluri. An insightful session on Pharmaco economics of cancer drugs – can we afford it?” was presented by Dr. Satheesh Kathula. “India’s unique value proposition towards Medical Tourism” was addressed by Mr. Shaaz Mehmood. The much-anticipated Women’s Leadership Forum featured extraordinarily successful Women Leaders representing a diversity of professions, involving public, private and government organizations.
The much-anticipated Women’s Leadership Forum featured extraordinarily successful Women Leaders representing a diversity of professions, involving public, private and government organizations. Medical Education & Research was led by Dr. Lokesh Eadara, Dr. P.V. Sudhakar, and Dr. G. Butchiraju. Community Outreach Program – HPV Vaccination at the Mahatma Gandhi Cancer Hospital, Visakhapatnam was coordinated by Dr. Syed Ahmed, Dr. Murali Krishna Voona, Dr. Meher Bala Medavaram, Secretary of AAPI.
Medical Education & Research was led by Dr. Lokesh Eadara, Dr. P.V. Sudhakar, and Dr. G. Butchiraju. Community Outreach Program – HPV Vaccination at the Mahatma Gandhi Cancer Hospital, Visakhapatnam was coordinated by Dr. Syed Ahmed, Dr. Murali Krishna Voona, Dr. Meher Bala Medavaram, Secretary of AAPI.

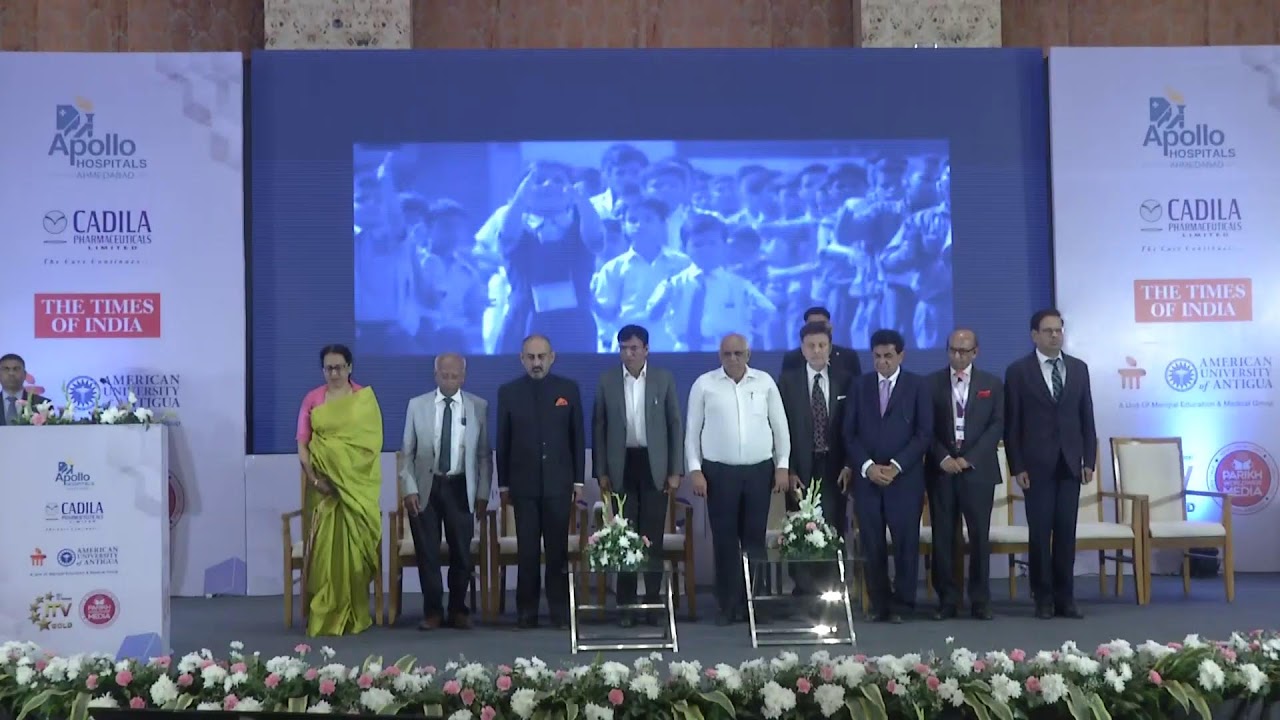
 Dr Ravi Kolli, President of AAPI, while describing the objectives of the Summit, said, “The Global Healthcare Summit has served as a means to raising awareness on key health care issues affecting the Indian subcontinent, such as the Stigma of Mental illness, Suicide prevention, Diabetes, Cardiovascular Diseases, Women’s and Children’s Health, Blindness Prevention and Hepatitis etc. Highlight of this Summit was to reaffirm NRI Physicians’ commitment towards improving health care and create model programs for management of various diseases and to improve outcomes universally, he added.
Dr Ravi Kolli, President of AAPI, while describing the objectives of the Summit, said, “The Global Healthcare Summit has served as a means to raising awareness on key health care issues affecting the Indian subcontinent, such as the Stigma of Mental illness, Suicide prevention, Diabetes, Cardiovascular Diseases, Women’s and Children’s Health, Blindness Prevention and Hepatitis etc. Highlight of this Summit was to reaffirm NRI Physicians’ commitment towards improving health care and create model programs for management of various diseases and to improve outcomes universally, he added. In addition, AAPI has plans to collaborate with various state and federal government programs to enhance the quality of healthcare delivery, making it affordable, efficient, and equitable, improving health outcomes universally and training the trainer sessions involving learning modules in different specialties, and tele-consultations.
In addition, AAPI has plans to collaborate with various state and federal government programs to enhance the quality of healthcare delivery, making it affordable, efficient, and equitable, improving health outcomes universally and training the trainer sessions involving learning modules in different specialties, and tele-consultations. Chief Guest at the Summit, Smt. Vidadala Rajini, Honorable Minister for Health, Family Welfare & Medical Education of state of Andhra Pradesh, said, “The Global Healthcare Summit is an important opportunity for all the healthcare professionals to learn from each other and enhance fellowship. I’m grateful to have this opportunity to attend and learn from all of you,” she said. “I believe that by working with you, we can improve the health and wellbeing of the people in the state. The government has the ability to design the best policies on healthcare, while delivering the best treatments and medical care to the patient is essentially in the hands of the physicians.” Among others who addressed the AAPI delegates and joined the felicitation of AAPI delegates and the local organizers of the Summit included, Shri. Gudivada Amarnath, Honorable Minister for IT.
Chief Guest at the Summit, Smt. Vidadala Rajini, Honorable Minister for Health, Family Welfare & Medical Education of state of Andhra Pradesh, said, “The Global Healthcare Summit is an important opportunity for all the healthcare professionals to learn from each other and enhance fellowship. I’m grateful to have this opportunity to attend and learn from all of you,” she said. “I believe that by working with you, we can improve the health and wellbeing of the people in the state. The government has the ability to design the best policies on healthcare, while delivering the best treatments and medical care to the patient is essentially in the hands of the physicians.” Among others who addressed the AAPI delegates and joined the felicitation of AAPI delegates and the local organizers of the Summit included, Shri. Gudivada Amarnath, Honorable Minister for IT. Describing some of the objectives of the GHS, Dr. Prasad Chalasani, Chair of GHS (USA) 2023 said. “We have tried to create an intellectually charged platform for experts to share their knowledge and experiences on some of the common professional issues that remain a challenge in spite of all the advances. The exchange of expertise and transfer of technology by the best brains is bound to offer positive and innovative solutions to some of the problems faced by humankind.”
Describing some of the objectives of the GHS, Dr. Prasad Chalasani, Chair of GHS (USA) 2023 said. “We have tried to create an intellectually charged platform for experts to share their knowledge and experiences on some of the common professional issues that remain a challenge in spite of all the advances. The exchange of expertise and transfer of technology by the best brains is bound to offer positive and innovative solutions to some of the problems faced by humankind.” AAPI, in collaboration with the AAPI India Foundation administered free HPV vaccines to over 100 low income young women from several government schools in the region, during a special launch and awareness camp organized at the Mahatma Gandhi Cancer Hospital, Visakhapatnam in India on Saturday, January 7th, 2023 with the objective of creating awareness and preventing cervical cancer, a leading cause of cancer deaths among women in India.
AAPI, in collaboration with the AAPI India Foundation administered free HPV vaccines to over 100 low income young women from several government schools in the region, during a special launch and awareness camp organized at the Mahatma Gandhi Cancer Hospital, Visakhapatnam in India on Saturday, January 7th, 2023 with the objective of creating awareness and preventing cervical cancer, a leading cause of cancer deaths among women in India. Dr. Udaya Shivangi, Chair of AAPI’s Women’s Committee, in her opening remarks provided an overview of the Forum and the many initiatives by the Forum both in India and the United States. Shri. MVV Satyavathi, Member of Parliament, representing Anakapalli was the Guest of Honor at the Women’s Forum. In her address, she congratulated AAPI, whose members having been born and educated in India, settled down in the US with success, have come back to India to serve the people of India and work together for the betterment of humanity.
Dr. Udaya Shivangi, Chair of AAPI’s Women’s Committee, in her opening remarks provided an overview of the Forum and the many initiatives by the Forum both in India and the United States. Shri. MVV Satyavathi, Member of Parliament, representing Anakapalli was the Guest of Honor at the Women’s Forum. In her address, she congratulated AAPI, whose members having been born and educated in India, settled down in the US with success, have come back to India to serve the people of India and work together for the betterment of humanity. The women leaders of AAPI dazzled on stage with elegance, and showcasing their talents by presenting two amazing Fashion Shows on Friday and Saturday at the Summit to the delight of the AAPI delegates.
The women leaders of AAPI dazzled on stage with elegance, and showcasing their talents by presenting two amazing Fashion Shows on Friday and Saturday at the Summit to the delight of the AAPI delegates.




























































 All women experience menopause differently, and many women experience changes in their sex life as they go through menopause. The loss of estrogen and testosterone following menopause induces multiple changes in a woman’s body and influences sexual function. Also, lower levels of estrogen can cause a drop in blood supply to the vagina, which can affect vaginal lubrication, causing the vagina to be too dry for comfortable sex. Moreover, other menopausal symptoms like bladder control problems, sleep disturbances, depression or anxiety, stress, medications, and other health concerns also affect the sexual well-being of the women experiencing menopause.
All women experience menopause differently, and many women experience changes in their sex life as they go through menopause. The loss of estrogen and testosterone following menopause induces multiple changes in a woman’s body and influences sexual function. Also, lower levels of estrogen can cause a drop in blood supply to the vagina, which can affect vaginal lubrication, causing the vagina to be too dry for comfortable sex. Moreover, other menopausal symptoms like bladder control problems, sleep disturbances, depression or anxiety, stress, medications, and other health concerns also affect the sexual well-being of the women experiencing menopause.
 The gala began with Dr. Uma Johnnalagadda, President of GAPI, Dr. Sreeni Ganagasani, and Dr. Raghu Lolabhattu, welcoming community members, family, friends, colleagues, and sponsors. “We, the AAPI-GAPI team worked hard to stick to the mission of AAPI, for education and charity to serve humanity. We thank each and every member that attended and supported the event. Our special thanks to all our Sponsors,” Dr. Jonnalagadda said.
The gala began with Dr. Uma Johnnalagadda, President of GAPI, Dr. Sreeni Ganagasani, and Dr. Raghu Lolabhattu, welcoming community members, family, friends, colleagues, and sponsors. “We, the AAPI-GAPI team worked hard to stick to the mission of AAPI, for education and charity to serve humanity. We thank each and every member that attended and supported the event. Our special thanks to all our Sponsors,” Dr. Jonnalagadda said. 



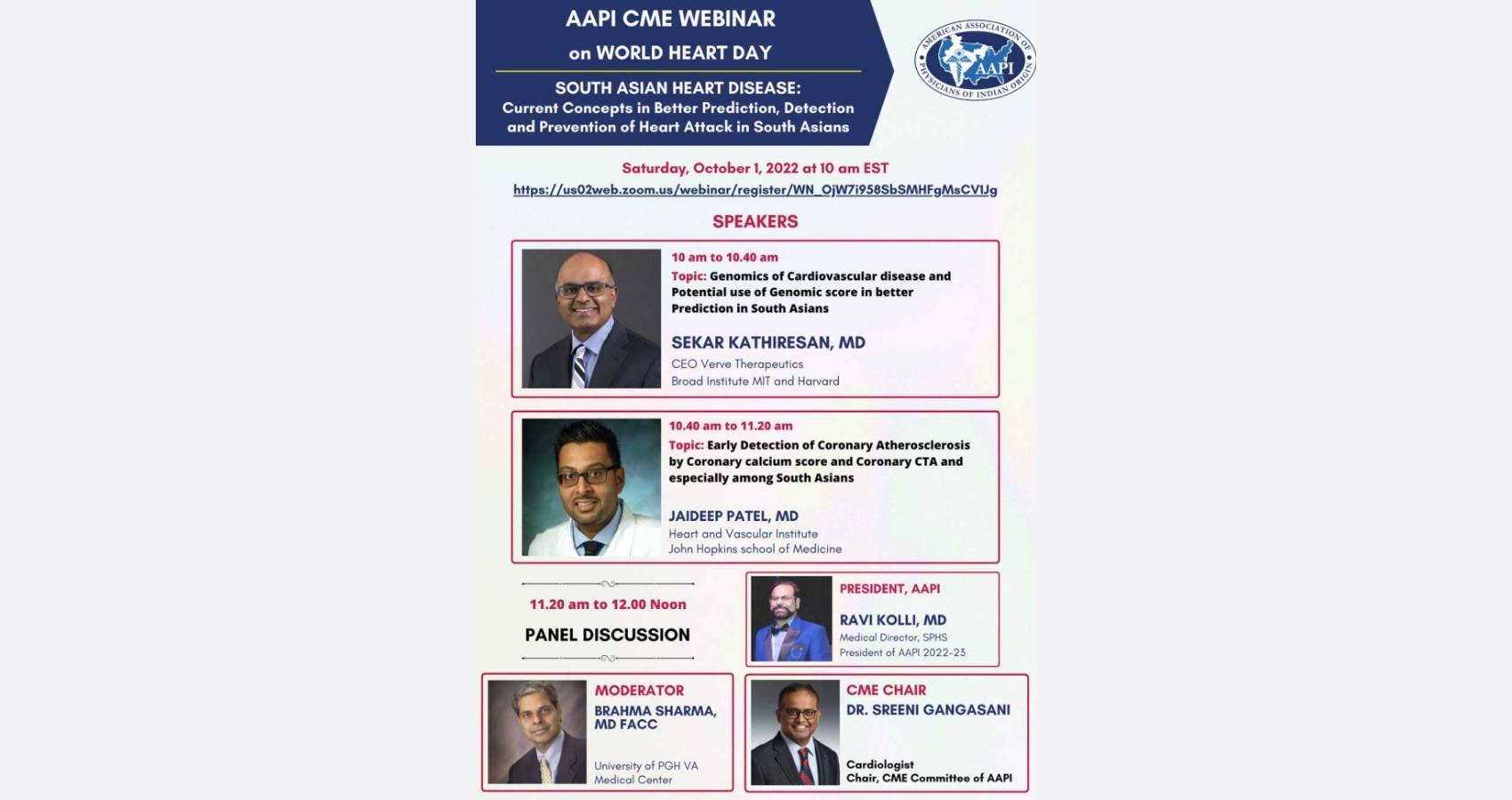
 In his remarks, Dr. Ravi Kolli, President of AAPI, said,” In the context of World Heart Day on September 29th, today’s conference is being organized to educate and create awareness about the major health issue faced by South Asians and offer ways to mitigate heart disease. Dr. Kolli said, “Today’s CME is focused on Recent Advances in South Asian Heart Disease by 2 eminent Indian American physicians who are in the forefront of research and treatment of this deadly disease. It is forward-looking information focusing on cutting edge technologies that can alter the treatment from chronic care model to once and done type of innovative therapies and latest recommendation for actively screening and offering early preventive care to treat cardiovascular disease, especially among the South Asians.”
In his remarks, Dr. Ravi Kolli, President of AAPI, said,” In the context of World Heart Day on September 29th, today’s conference is being organized to educate and create awareness about the major health issue faced by South Asians and offer ways to mitigate heart disease. Dr. Kolli said, “Today’s CME is focused on Recent Advances in South Asian Heart Disease by 2 eminent Indian American physicians who are in the forefront of research and treatment of this deadly disease. It is forward-looking information focusing on cutting edge technologies that can alter the treatment from chronic care model to once and done type of innovative therapies and latest recommendation for actively screening and offering early preventive care to treat cardiovascular disease, especially among the South Asians.”  Dr. Jaideep Patel is a cardiologist in Baltimore, Maryland and is affiliated with multiple hospitals in the area, including at the Heart & Vascular Center at Johns Hopkins University, with primary focus on Preventive Cardiology, pointed out that usual risk scoring has been done on Caucasians and cannot be extrapolated to south Asians. Citing Multiethnic Study of Atherosclerosis, that he was part of Dr. Patel said,
Dr. Jaideep Patel is a cardiologist in Baltimore, Maryland and is affiliated with multiple hospitals in the area, including at the Heart & Vascular Center at Johns Hopkins University, with primary focus on Preventive Cardiology, pointed out that usual risk scoring has been done on Caucasians and cannot be extrapolated to south Asians. Citing Multiethnic Study of Atherosclerosis, that he was part of Dr. Patel said, 
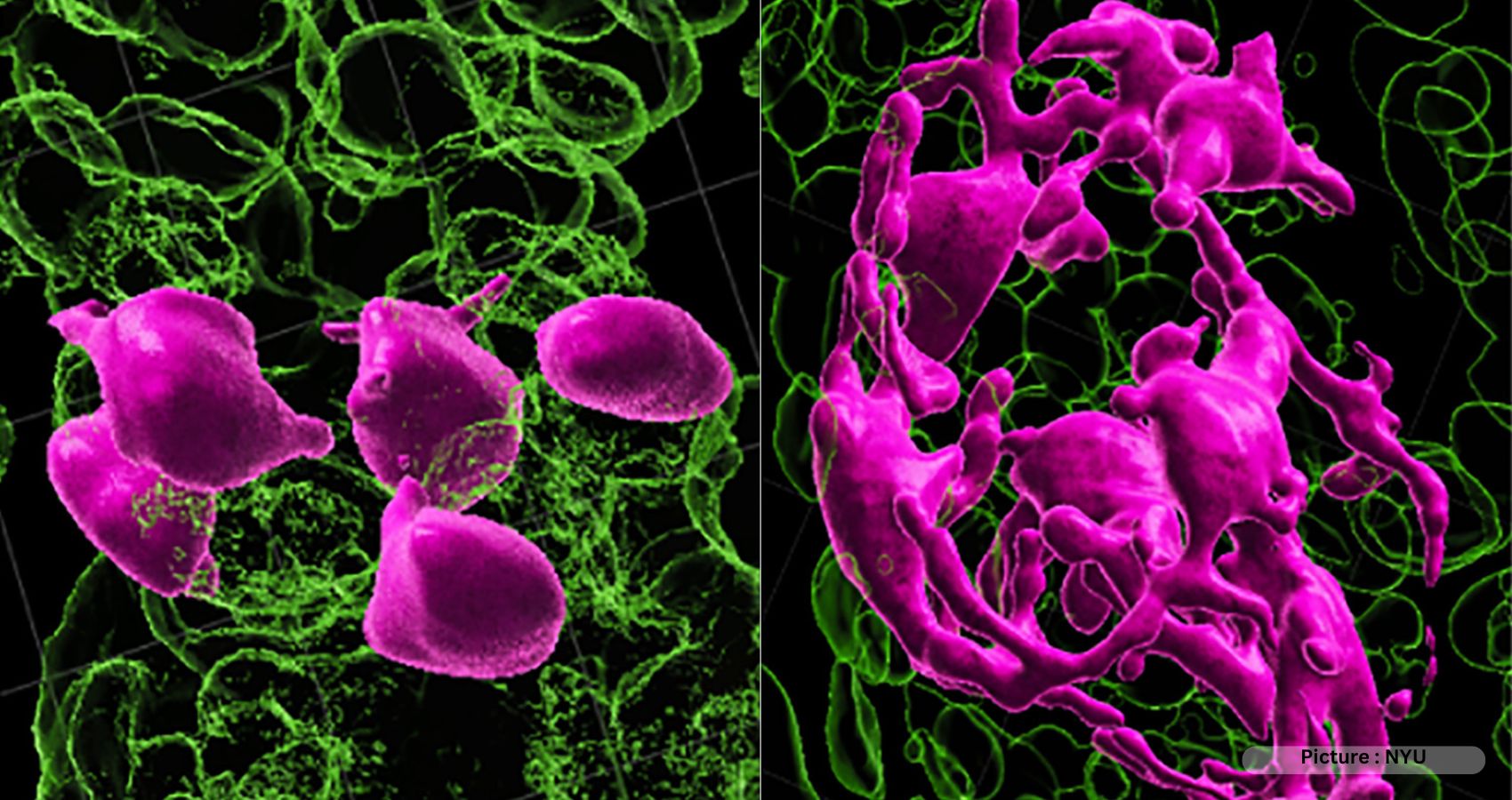
 The new study, published Friday (Sept. 30) in the journal
The new study, published Friday (Sept. 30) in the journal 







