Indian American women face rising breast cancer risks, often overlooked due to cultural barriers and a lack of disaggregated health data, as illustrated by the experiences of women like Srila.
During the early days of the pandemic, Srila, a healthcare professional in the Bay Area, discovered a lump in her breast. “While showering, I used to feel a little bit of something tough, but I didn’t pay much attention,” she recalled.
Having lived in the U.S. for over 20 years and balancing her career with family responsibilities, Srila was due for her biennial mammogram in 2020. However, as the world shut down and daily anxieties mounted, she found it difficult to prioritize what seemed like a non-urgent health issue. Instead, she focused on running fundraisers for a Bay Area nonprofit she co-founded to send critical pandemic supplies to India.
“I’m normally a very attentive and science-driven person, but there was so much chaos with the pandemic going on,” she said.
By August 2020, the grape-sized lump and persistent tightness in her breast could no longer be ignored. Upon contacting her primary care physician, she was urged to come in immediately. At 47, Srila was unaware of the alarming trend: breast cancer rates among Asian American women under 50 were rising significantly.
According to a 2024 report from the American Cancer Society, Asian American and Pacific Islander (AAPI) women experienced the fastest-growing breast cancer incidence of any racial or ethnic group between 2012 and 2021, with a rise of 2.6% per year. Dr. Lihua Liu, a professor at the University of Southern California, noted that cancer was once seen as a disease primarily affecting the elderly, but statistics indicate a troubling shift. Between 2000 and 2021, new breast cancer cases among AAPI women under 50 surged by 52%.
Moreover, a 2019 CDC study found that immigrant Asian women faced a two- to three-fold higher risk of developing breast cancer compared to their U.S.-born counterparts, even after accounting for known risk factors such as reproductive history and family history. The reasons for this elevated risk among women arriving from Asia remain unclear.
For Indian American women like Srila, the situation is even more complex due to the lack of disaggregated data on South Asian communities. This absence makes it difficult to fully understand the scope of their risk.
Dr. Liu emphasized that closer studies reveal significant differences in screening rates, stage at diagnosis, treatment, and health outcomes among various Asian groups. Census data often lumps together individuals from diverse backgrounds, including Indian, Pakistani, Nepalese, and Sri Lankan, obscuring the specific trends affecting South Asian populations. Despite being the second-largest Asian group in the U.S. with a median age of 34, Indian Americans have received less attention regarding their increasing breast cancer risk compared to other health issues like heart disease and diabetes.
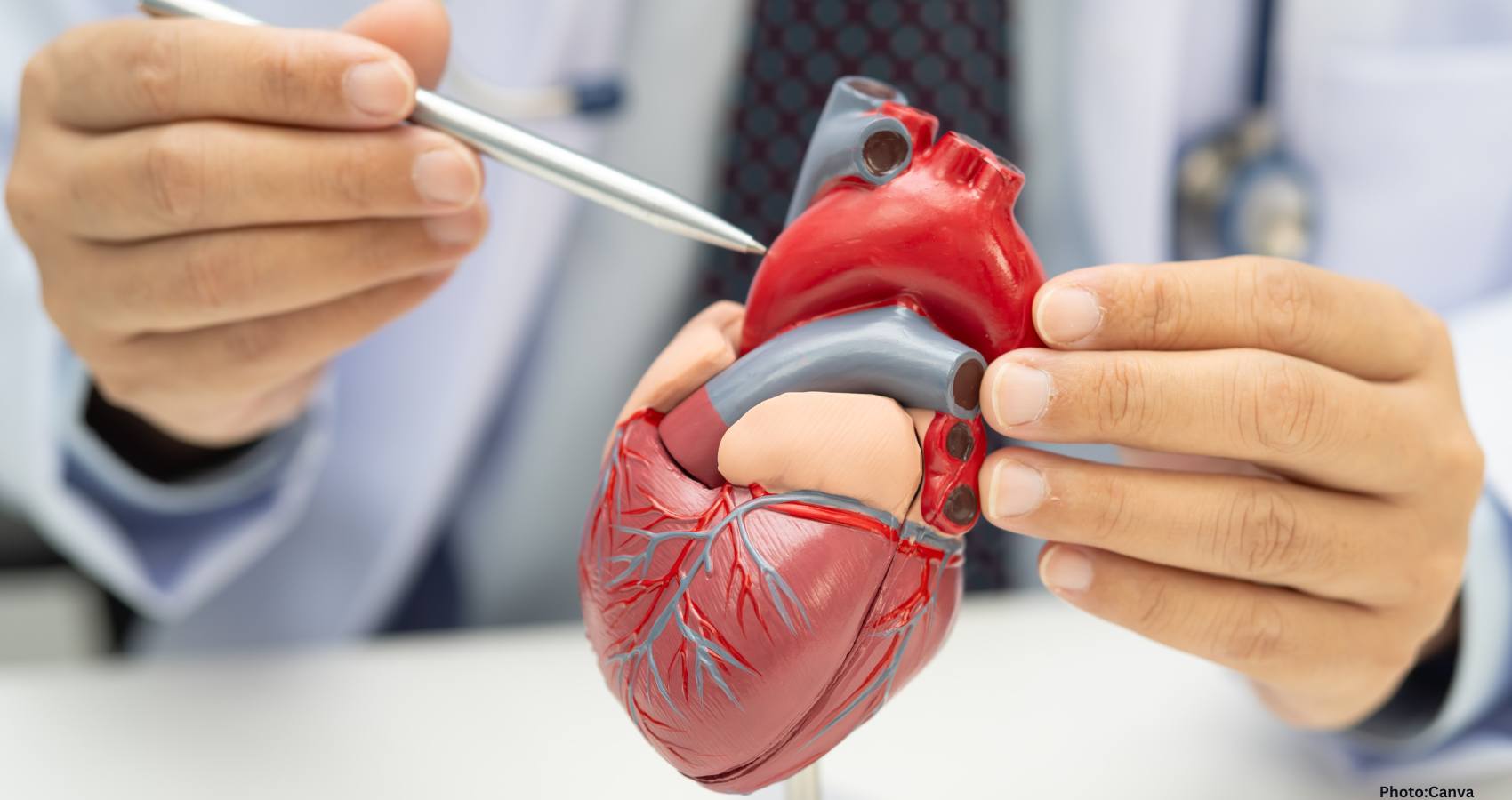
Dr. Preeti Farmah, a breast surgical oncologist at El Camino Health, explained that breast cancer risk factors can be inherited or genetic, but they are also influenced by lifestyle and environmental factors. For immigrant Asian American women, the process of westernization plays a crucial role in shaping these risks.
As Asian Americans adopt American lifestyles, they often experience changes in diet, reproductive practices, and environmental exposures that increase their vulnerability to breast cancer. Dr. Farmah noted that adopting a westernized lifestyle can lead to higher obesity rates, declining fertility rates, and a tendency to have children later in life. These factors extend the body’s total window of estrogen exposure, modestly increasing breast cancer risk.
Additionally, the demands of balancing careers and family life in the U.S. often result in fewer pregnancies and shorter breastfeeding durations, further compounding the risk. Chronic stress can also elevate cortisol levels, which may contribute to increased breast cancer risk.
Dr. Farmah explained that estrogen acts as a fuel for cancer cells. As dietary habits shift toward higher fat and processed foods, combined with reduced physical activity, obesity becomes a significant risk factor. “When you have fatty tissue, it can also produce estrogen,” she added.
Dense breast tissue, which disproportionately affects AAPI women, complicates detection. Both small breast cancers and dense tissue appear white on mammograms, making them harder to identify. Dr. Farmah noted that this increases the likelihood of undetected cancers, as subtle signs may remain hidden.
Cultural barriers also play a significant role in preventive care. Many first-generation Asian Americans delay seeking preventive care due to health care norms from their home countries, where visits to doctors typically occur only when one is ill. Dr. Harpreet Pannu, a Kaiser internist in San Jose, explained that this mindset can hinder participation in preventive health measures.
A Rutgers study of Indian and Pakistani women in the U.S. linked poor mammogram screening rates to lifestyle and cultural factors, including lack of family support, transportation issues, modesty concerns, and beliefs about cancer as divine punishment. With two-thirds of Indian Americans born outside the U.S., these cultural norms significantly influence their approach to mammograms.
According to the CDC, AAPI women aged 40 to 49 have among the lowest mammography rates of any racial group, with only 54% reporting a mammogram in the past two years, compared to 60% of White women.
As immigrant women navigate a new culture and healthcare system while balancing work and family, preventive care often falls by the wayside.
However, early detection can lead to better outcomes. Nibedita, a Los Angeles resident, had her first mammogram at 40, which was negative. A few months later, during a self-exam, she discovered a lump. Her doctor quickly referred her for an ultrasound and biopsy, leading to a diagnosis of triple-negative breast cancer (TNBC), an aggressive form of the disease that occurs at higher rates in women of Indian subcontinent ancestry than in White women. Fortunately, her cancer was caught early, allowing her to undergo successful treatment.
Srila’s journey took a similar turn after her initial consultation. Within days, an ultrasound and needle biopsy confirmed a triple-positive breast cancer diagnosis. Following conflicting treatment recommendations, she sought a second opinion from a Stanford oncologist, who advised chemotherapy before surgery. Despite the challenges of undergoing treatment during the pandemic, Srila persevered through six cycles of chemotherapy, followed by surgery and radiation.
Tragically, her cancer metastasized to her brain, leading to multiple tumors. The experience highlighted the differences in follow-up care protocols between the U.S. and India, where full-body scans are more common after treatment.
Despite the setbacks, Srila remains determined. “I don’t want to live to breathe. I want to live to live,” she said, emphasizing her desire to continue pursuing her passions. She is currently undergoing active treatment and monitoring, benefiting from specialized care and advanced medical technology.
This article was produced in partnership with the USC Annenberg Center for Health Journalism’s “Healing California” Ethnic Media Collaborative.


















































































 “We received 238 Stem Donors who registrations at our Stem Donor Registry during the Global Healthcare Summit held in Bhubaneshwar, Orissa from Jan 9-11, 2026,” said Dr. Sashi Kuppala, Chair of the Stem Cell Drive. “ To put it in context, we would have had to do 20 drives to get those many registrations in the United States. Thanks to Dr. Amit Chakrabarthy, we successfully launched the project in India.”
“We received 238 Stem Donors who registrations at our Stem Donor Registry during the Global Healthcare Summit held in Bhubaneshwar, Orissa from Jan 9-11, 2026,” said Dr. Sashi Kuppala, Chair of the Stem Cell Drive. “ To put it in context, we would have had to do 20 drives to get those many registrations in the United States. Thanks to Dr. Amit Chakrabarthy, we successfully launched the project in India.” During the inaugural ceremony of GHS, Prof. R C Das, Dean and Principal of KIMS stressed the importance and urged the medical students at KIM to come forward and register for Stem Donorship. The students were then led to pledge and commit to encourage Stem Donorship among the patient population they are committed to serve.
During the inaugural ceremony of GHS, Prof. R C Das, Dean and Principal of KIMS stressed the importance and urged the medical students at KIM to come forward and register for Stem Donorship. The students were then led to pledge and commit to encourage Stem Donorship among the patient population they are committed to serve. Stem cells are one of the treatment options for certain types of cancers. HLA typing, based on which stem cell donors and patients are matched is ethnicity specific. Indian patients have higher chances of matching with Indian donors. Unfortunately, Indian donor pool is very limited, making it difficult for patients to find a proper match. Moreover, until now, patients and their families are doing these drives on their own to find the match in addition to dealing with the diagnosis. There has been no unified push to increase the Indian donor pool.
Stem cells are one of the treatment options for certain types of cancers. HLA typing, based on which stem cell donors and patients are matched is ethnicity specific. Indian patients have higher chances of matching with Indian donors. Unfortunately, Indian donor pool is very limited, making it difficult for patients to find a proper match. Moreover, until now, patients and their families are doing these drives on their own to find the match in addition to dealing with the diagnosis. There has been no unified push to increase the Indian donor pool. Dr. Hetal Gor, Chair of AAPI BOT, emphasized the need for commitment. She said, “You could be someone’s only match—their only hope. Registering is a serious promise, but the donation process is safe and complication-free.”
Dr. Hetal Gor, Chair of AAPI BOT, emphasized the need for commitment. She said, “You could be someone’s only match—their only hope. Registering is a serious promise, but the donation process is safe and complication-free.” Dr. Krishan Kumar, Vice President-Elect, while highlighting the disparity, said, “70% of patients lack a family match. For Indians, the odds are even lower due to the limited donor pool.”
Dr. Krishan Kumar, Vice President-Elect, while highlighting the disparity, said, “70% of patients lack a family match. For Indians, the odds are even lower due to the limited donor pool.” Dr. Sashi Kuppala, while explaining the science, said, Matching donors is based on HLA typing, which is inherited and ethnicity-specific. Thousands of patients rely on transplants to survive.” Dr. Kuppala pointed to the “tremendous response to this initiative from the AAPI members and the wider Indian community.”
Dr. Sashi Kuppala, while explaining the science, said, Matching donors is based on HLA typing, which is inherited and ethnicity-specific. Thousands of patients rely on transplants to survive.” Dr. Kuppala pointed to the “tremendous response to this initiative from the AAPI members and the wider Indian community.”







