Forbes has recognized 11 Indian Americans in its “250 America’s Greatest Innovators” list, highlighting their significant contributions to technology and medicine as the nation celebrates its 250th anniversary.
Forbes recently unveiled its “250 America’s Greatest Innovators” list to commemorate the United States’ 250th anniversary, showcasing a diverse group of visionary founders and executives who are reshaping global technology and medicine. Among the honorees are 11 Indian Americans, whose groundbreaking work spans from the early days of the internet to the cutting-edge developments in generative AI.
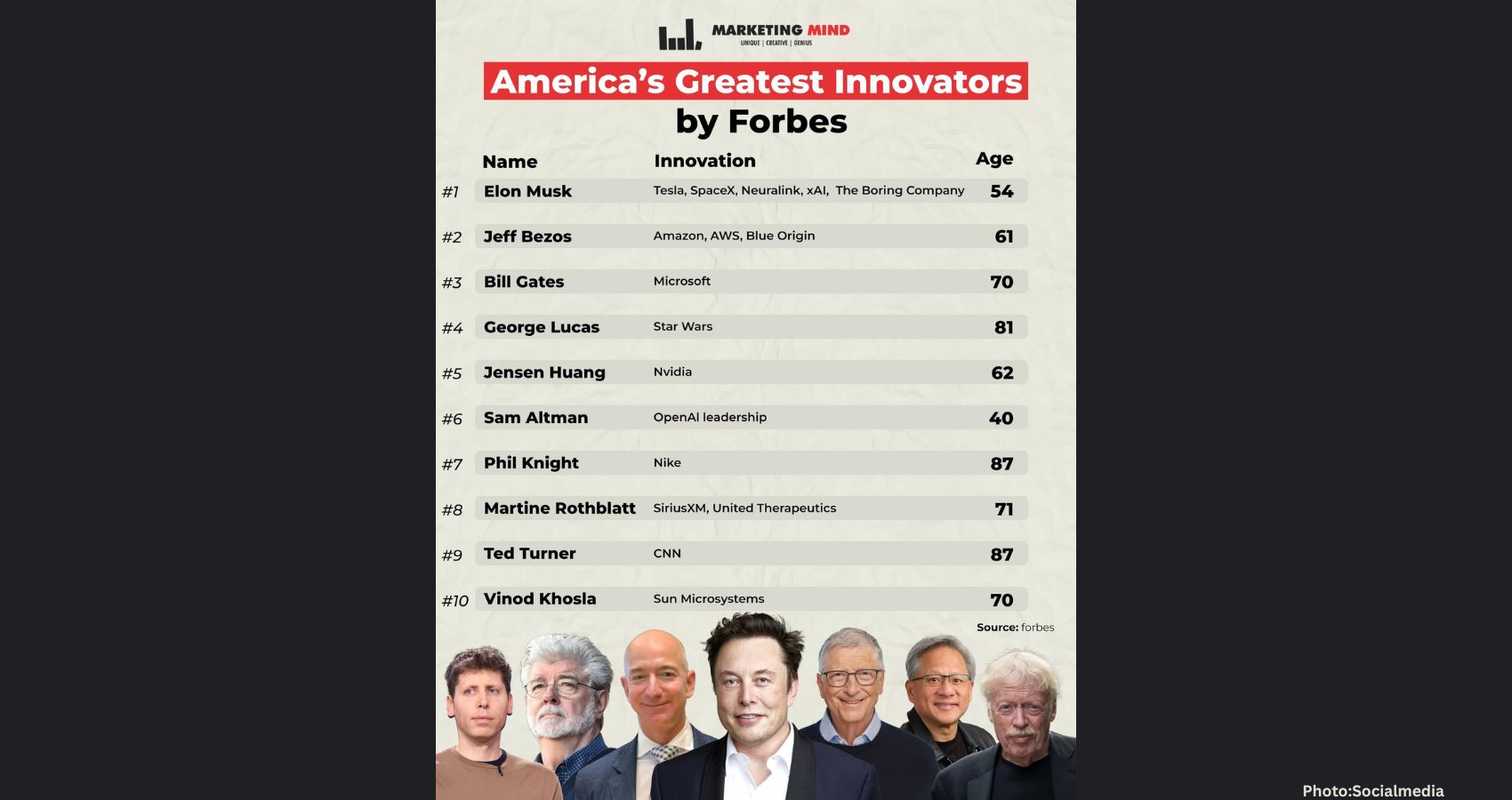
Leading this distinguished group is Vinod Khosla, co-founder of Sun Microsystems and a prominent venture capitalist, who secured the No. 10 spot. Khosla is renowned for his “black swan” investing style, with early investments in OpenAI and green technology solidifying his reputation as a leading risk-taker in the industry.
Close behind Khosla are tech giants Satya Nadella and Sundar Pichai, who have been instrumental in “re-founding” Microsoft and Alphabet, respectively. Their leadership has pivoted these legacy companies toward an AI-first future, reflecting the transformative power of innovation in the tech landscape.
The Forbes list emphasizes that innovation is often a marathon rather than a sprint. Suma Krishnan, who ranks No. 127, has made significant strides in treating “butterfly skin” disease. She co-founded Krystal Biotech in her 50s to develop the first topical gene therapy, marking a pivotal moment in medical innovation.
Similarly, Jay Chaudhry, ranked No. 128, has been recognized for his pioneering work in “zero trust” cloud security at Zscaler, which has disrupted the traditional firewall industry and redefined security protocols in the digital age.
The Indian American diaspora continues to make substantial contributions to technical infrastructure. Neha Narkhede, co-founder of Confluent and now CEO of Oscilar, is celebrated at No. 155 for her work in real-time data streaming. At MIT, Sangeeta Bhatia, ranked No. 161, has been honored for her innovative approach to merging microchips with biology, revolutionizing drug testing methodologies.
The diversity of this group extends into the daily lives of millions. Aman Narang, who ranks No. 177, has transformed the restaurant industry with Toast’s management platform. Baiju Bhatt, at No. 183, has democratized retail investing through Robinhood and is now pivoting to space-based solar power with Aetherflux. Naval Ravikant, ranked No. 230, has broadened access to startup funding via AngelList, further contributing to the entrepreneurial ecosystem.
The final names on the list reflect a commitment to human equity and efficiency. Shiv Rao, ranked No. 235, has been recognized for his AI medical scribe, Abridge, which automates clinical documentation to alleviate physician burnout. Shan Sinha, at No. 202, has made significant contributions to data management and healthcare safety, while Shivani Siroya, ranked No. 238, has been lauded for her work with Tala, which utilizes mobile data to provide credit to the “unbanked” in emerging markets.
This impressive collection of 11 innovators underscores a robust pipeline of talent that has become essential to the American economy. Whether they began their journeys in a garage or now lead major conglomerates, these individuals have successfully transformed complex scientific and digital theories into everyday realities.
According to Forbes, the achievements of these innovators highlight the critical role that diverse perspectives play in driving progress and shaping the future.