(San Antonio, Tx. June 26, 2022) The historic 40th annual convention organized by the American Association of Physicians of Indian Origin (AAPI) concluded at the world-famous Riverwalk Henry B Gonzalez Convention Center in San Antonio in Texas on Saturday, June 25th, 2022 with a Gala Bollywood Nite, during which a new Leadership Team led by Dr. Ravi Kolli assumed charge of the four decades old premier Medical Organization, representing the strong and powerful 120,000 physicians of Indian heritage.
The four days long annual convention and scientific assembly, attended by over 10,000 AAPI delegates, while celebrating the achievements of the Indian American Physicians, focused on the theme, “Physician Heal Thyself” with several unique and first-of-a-kind opportunities to help AAPI members self-care, especially in the context of Covid related physicians burn out, paid tributes and celebrated freedom and democracy, honoring India and its 75 years of Independence Day celebrations- co-sponsored by the Embassy of India & the Consulate General of India (CGI) – Houston.
“AAPI’s strength is its numbers and members. Our Sakthi is in our Samkhya and our Sabhyas,” Dr. Ravi Kolli stated in his inaugural address immediately after he assumed charge as the 41st President of AAPI. “You are that powerful threads of this colorful and strong fabric, and your participation and contributions are essential for its continued success. So, thank you all,” Dr. Kolli told AAPI delegates and distinguished guests who had packed the Ball Room at the Henry Gonzalez Convention Center during the Presidential Gala.
Dr. Kolli will work with Dr. Anjana Sammadar, President-Elect; Dr. Satheesh Kathula, Vice President; Dr. Meherbala Medavaram, Secretary and Dr. Sumul Raval, Treasurer of AAPI for the year 2022-23. Dr. V. Ranga will serve as the Chair, AAPI Board of Trustees. Giving representation and strengthening the voice of young physicians of Indian origin, Dr. Pooja Kinkhabwala will serve as the President, AAPI Young Physicians Section (YPS) and Dr. Ammu Susheela is the President of AAPI- Medical Student/Residents & Fellows Section (MSRF). Dr. Anupama Gotimukula will serve as the Immediate Past President of AAPI.
 Dr. Anupama Gotimukula, the Immediate Past President of AAPI said, “Our leadership team has worked diligently on so many wonderful projects and activities including educational, philanthropic, legislative, networking, and many more activities benefitting our members and communities. This has been possible because of the incredible work and support from the dedicated team of leaders, members, and our supporting office staff,” the only 4th woman President of AAPI in the four decades long history of AAPI, said.
Dr. Anupama Gotimukula, the Immediate Past President of AAPI said, “Our leadership team has worked diligently on so many wonderful projects and activities including educational, philanthropic, legislative, networking, and many more activities benefitting our members and communities. This has been possible because of the incredible work and support from the dedicated team of leaders, members, and our supporting office staff,” the only 4th woman President of AAPI in the four decades long history of AAPI, said.
“Our physician members have worked very hard during the covid 19 pandemic. The 2022 convention is a perfect time to heal the healers with a special focus on wellness,” said Dr. Jayesh Shah, Chair of AAPI Convention 2022. Dr. Shah praised the dedication and generosity of each member for giving their best, to make this Convention truly a memorable one for every participant.
Put together by a highly talented and dedicated team of Convention Committee members, the convention was filled with programs and activities that cater to the body, mind and soul. The Convention was a unique experience for everyone, Dr. Sathessh Kathula, Secretary of AAPI said.
During the BOT luncheon chaired by Dr. Kusum Punjabi, the youngest ever to hold the position, handed over the office to the new Chair, Dr. Vishweshwar R. Ranga. In her address, Dr. Punjabi highlighted the many initiatives under her leadership. She said, “The Board of Trustees this year has launched the AAPI Medical Project Grant (MPG). The purpose of this grant is to financially support AAPI medical students/residents/fellows/young physicians in various medical projects such as observerships, community service projects, entrepreneurships, innovation developments, etc.:
 Dr. V. Ranga in his address he said, “My goal in the coming year is to formalize and create AAPI leadership academy working with executives from American College of Physicians for the development of leadership roles for all AAPI members. I want to work hard to engage young physicians and attract them to AAPI. They are the future of AAPI.”
Dr. V. Ranga in his address he said, “My goal in the coming year is to formalize and create AAPI leadership academy working with executives from American College of Physicians for the development of leadership roles for all AAPI members. I want to work hard to engage young physicians and attract them to AAPI. They are the future of AAPI.”
Dr. Surender Purohit, Chair of AAPI’s Charitable Foundation provided a brief summary of the many initiatives AAPI has undertaken in recent years, especially benefitting the remotest villages in the country.
Welcoming AAPI delegates to San Antonio, Ron Nirenberg, Mayor of San Antonio, declared June 24th as AAPI Day and International Yoga Day in the City of San Antonio. While praising AAPI and its members for their contributions, Nirenberg said, “We are honored to host the largest gathering of Indian American physicians in our vibrant city, home to some of the best healthcare facilities in the nation.”
AAPI delegates had a rare glimpse to the rich cultural heritage of India through a video presentation depicting the unique diversity of India and a variety of mesmerizing performances of Indian/Mexican Fusion Dances, ranging from Bharatnatyam, folk dances, and the traditional Indian dances in sync with Mexican pop dances, which were a treat to the hearts and souls of everyone. National Spieling Bee Champion 2022 Harini Logan was recognized during the convention Gala.
 In his keynote address, Ambassador Taranjit Singh Sandhu lauded the several initiatves of AAPI over the past four decades and said, “Over the past four decades, AAPI has been doing an outstanding job in advocacy and health education. You play an important role, especially during the Covid Pandemic/” Speaking at length on the growing Indo-US relationship, the veteran diplomat said, “Over the last two decades, India and the United States have overcome the hesitations of history and fashioned a remarkable partnership, built on a bipartisan consensus in the U.S. and cross-party support in India.” Elaborating on the collaboration between India and the US, he said, “From the provision of active pharmaceutical ingredients to generic medicines that have lowered drug prices and created jobs and investments, India has demonstrated its reliability as a supply chain partner, especially as de-risking from single country supplies has become a priority.”
In his keynote address, Ambassador Taranjit Singh Sandhu lauded the several initiatves of AAPI over the past four decades and said, “Over the past four decades, AAPI has been doing an outstanding job in advocacy and health education. You play an important role, especially during the Covid Pandemic/” Speaking at length on the growing Indo-US relationship, the veteran diplomat said, “Over the last two decades, India and the United States have overcome the hesitations of history and fashioned a remarkable partnership, built on a bipartisan consensus in the U.S. and cross-party support in India.” Elaborating on the collaboration between India and the US, he said, “From the provision of active pharmaceutical ingredients to generic medicines that have lowered drug prices and created jobs and investments, India has demonstrated its reliability as a supply chain partner, especially as de-risking from single country supplies has become a priority.”
Aseem Mahajan, Consul General of India in Houston, referred to the significance of “India and the United States, the two most vibrant democracies, representing two great multicultural societies with shared values, who are natural partners” working together in several areas of interest to both the nations.
Dr. Jack Resneck, President of American Medical Association praised the contributions and achievements of Indian American physicians, who serve and provide best healthcare to every 7th patient in the United States. “It’s time our nation renews our commitment to you for the incredible services you provide to our nation,” he said. During a Plenary session, he provided a detailed description of the many steps AMA has been undertaking to root out the causes for physician burn out and enhance healthcare delivery in the nation through education and advocacy at the state and national levels.
Keynote speaker, Little Master Sunil Gavaskar was introduced by Venky Adivi, Chief Executive Officer of the Convention. Gavaskar, a record holder of numerous international Cricket matches, in his address said, “Yours is the greatest of all professions in the world. You have put your lives at risk during the Pandemic to save the lives of others. Yours is the noble profession that I have admired always.”
Dr. Rahul Gupta, the nation’s “drug czar” and top drug policy official, while conveying the greetings from President Joe Biden and Vice President Kamala Harris praised the contributions of Indian American Physicians. “The role of the Drug Czar has never been as critical as it’s today,” he told the AAPI delegates, who have been advocating for prize control of drugs to contain overall healthcare costs. “AS physicians of Indian Origin, we have learnt to find simple solutions to complex problems. We need 21st century solutions to 21st century problems.” And he encouraged his colleagues to think and find ways to make a difference in the healthcare delivery in the country.
Others who addressed the Convention included Dr. Bobby Mukamala, Chair of BOT at American Medical Association, Congressman Joaquin Castro from Texas, and Peter Jay Hortez,, who was part of the plenart session on “Covid Vaccination Globally and Vaccine Hesitancy.”
In her spiritual discourse, Sadhvi Bhagawati Saraswati, PhD, Spiritual leader, teacher and author, while pointing to how we are creating a vicious negative health through fear, stress and anxiety in this country, her message today was to focus on the Synonym for HEALTH: Health, Embrace, Allow, Love, Time for yourself, and Help others.
In his live video message, Paramaguru Sharath Jois, Lineage holder of Ashtanga Yoga, told AAPI leaders as to how “each of you have sacrificed your life. I congratulate the organizers for focusing on heal the healers and using Yoga our traditional method to help us in our daily lives.” Referring to the 7th anniversary of India’s Independence he said, “It must help us transcend all that divide us on the basis of caste, creed and status.”
The much anticipated wellness package in collaboration with all the 10 City Council Districts of San Antonio, TX and Mayor Ron Nirenberg and iDoYoga San Antonio organized its flagship Free Yoga Classes and Education on the benefits and ways to make yoga a part of one’s daily life during the course of the entire convention. The convention was focused on themes such as how to take care of self and find satisfaction and happiness in the challenging situations they are in, while serving hundreds of patients everyday of their dedicated and noble profession.
Led by internationally famed yoga gurus, including Sadhvi Bhagawati Saraswati, PhD, Spiritual leader, teacher and author; Paramaguru Sharath Jois, Lineage holder of Ashtanga Yoga; and, Eddie Stern, Yoga teacher, speaker and author, the highly anticipated and popular Yoga on the famous Riverwalk was part of the global celebration of the 8th International Day of Yoga (IDY).
Some of the major themes at the convention included: Yoga and Meditation practices, Welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, Ailment based yoga therapy sessions, Workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine. Yoga gurus and experts leading the wellness sessions include Paramguru Sharatha Jois, Sadhvi Bhagawati, Saraswati Eddie Stern, Dr. Sat Bir Khalsa, Dr. Dilip Sarkar, Dr. Pankaj Vij, and Dr. Param Dedhia.
Dr. Anjana Sammadar, President-Elect , pointed out: “There was a sense of joy and relief on the faces of the over 1,000 physicians who have come together to celebrate their achievements, contributions, and to network and deepen their relationship even as the Covid Pandemic is waning and people are able to mingle freely and interact with one another cautiously.”
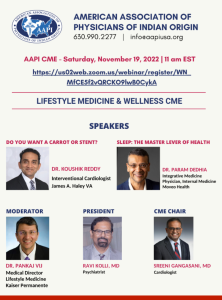
AAPI delegates attended a multidisciplinary CME conference that allowed specialists and primary care physicians to interact in an academic forum. World-renowned speakers discussed gaps between current and best practice of wide-ranging topics at the CME sessions.
Dr. Satheesh Kathula, Vice President of AAPI said, as many as CME credit hours have been provided by outstanding speakers all year and provided cutting edge CMEs to members. He thanked the Chicago Medical Society, Dr. Vemuri Murthy, Dr. Amit Chakraborty, CME Chair and Dr. Sagar Galvankar, & Co-Chair for their diligent efforts all the prominent speakers who shared their expertise with AAPI delegates.
Dr. Meherbala Medavaram said, some of the major events at the convention included: Workshops and hands-on sessions on well-being, 10-12 hours of CMEs, Women’s Forum, CEOs Forum, AAPI Got Talent, Mehfil, Bollywood Nite, Fashion Show, Medical Jeopardy, Poster/Research Contest, Alumni and Young Physicians events and Exhibition and Sale of Jewelry, Clothing, Medical Equipment, Pharma, Finance and many more.
According to Dr. Sumul Raval, the convention offered a venue for Physicians and healthcare professionals from across the country and internationally to convene and participate in the scholarly exchange of medical advances, to develop health policy agendas, and to encourage legislative priorities in the coming year.
The panelists at the prestigious Women’s Forum included: Dr. Juby A. Jacob-Nara, a Public Health Physician, Vice President and Head of Global Medical Respiratory Allergy & Gastroenterology (Sanofi-Genzyme); Dr. Kalpalatha Guntupalli, Endowed Professor for Pulmonary Disorders, Baylor College of Medicine; Dr. Sowjanya Mohan, Group Chief Medical Officer, Texas Group/Tenet Health; and, Ms. Rosemary Hickman, Semmes Foundation Education Manager at the Mcnay Art Museum.
The CEOs Forum moderated by Dr. Joseph Chalil had a panel of Industry Leaders including: Dr. Juby A Jacob-Nara, Vice President, Head of Global Medical- Sanofi-Genzyme; Robert Mattchione, from NOVA; Dr. Monika Kapur; Ms. Rebecca Seidel. Medtronix; and Mario Ball. A pioneering AAPI Medical Leadership Council is being formed to collaborate with Industry leaders and to be the voice of healthcare providers, said Dr. Chalil.
Mehfil gave AAPI members to showcase their skills. Dr. Satheesh Kathula in the incoming Vice President of API was declared the winner of the contest. During the popular Fashion Parade presented by world renowned fashion designer Archana Kochar had beautiful and handsome young men and women wearing handmade colorful apparel made by villagers in Madhya Pradesh, cat walked on the ramp.
 Dozens of local children from ages 8 to 16, trained by Yoga Masters in San Antonio by presenting and demonstrating multiple Yoga Aasanas to the tune of Vande Mataram provided valuable education on Yoga and its importance in life. Every evening the popular AAPI Got Talent and
Dozens of local children from ages 8 to 16, trained by Yoga Masters in San Antonio by presenting and demonstrating multiple Yoga Aasanas to the tune of Vande Mataram provided valuable education on Yoga and its importance in life. Every evening the popular AAPI Got Talent and
Each day of the convention had a specific theme. On Thursday, the theme chosen is “Unity in Diversity” and the delegates showcased one’s own state dress code. Heritage India was the theme for Friday honoring and celebrating India’s rich culture and diversity. On Saturday, the focus was on the much loved Bollywood with special performance by popular Bollywood singer Shaan, The cuisine served each will day match the theme chosen for each day.
Dr. Jagan Ailinani was honored with Life Time Achievement Award. The Distinguished Physician Award was given to Dr. Vijay Yeldandi and AAPI’s Most Distinguished Award was given to Dr. Ravindra Nathan. AAPI’s Most Distinguished YPS Award was given to Dr. Sejal Hathi and the AAPI’s Most Distinguished MSRF Award was given to Aaiswariya Gulani. r. Gotimukula honored Dr. Udaya Shivangi, Dr. Sujeeth Punnam, Dr. Dwarkanath Reddy and AAPI’s Legal Advisor with Presidential Awards for their dedication and support during her presidency.
“Welcome to Philadelphia for the 41st annual convention which will provide you all with extensive academic presentations, recognition of achievements and achievers, and professional networking at the al and evening social events,” Dr. Ravi Kolli announced. For more details, please visit: www.aapiconvention.org and www.aapiusa.org


 “The essence of AAPI is educational,” Dr. Kolli added. “That translates into numerous Continuing Medical Education (CME) and non-CME seminars by experts in their fields. The GHS 2023 with the theme of “True and Total Health is the Wellbeing of Mind, Body, and Spirit” has had several CME sessions that focused on Mental Health, Infant and Maternal Mortality as well as various other medical specialty updates, research, and Medical Jeopardy.”
“The essence of AAPI is educational,” Dr. Kolli added. “That translates into numerous Continuing Medical Education (CME) and non-CME seminars by experts in their fields. The GHS 2023 with the theme of “True and Total Health is the Wellbeing of Mind, Body, and Spirit” has had several CME sessions that focused on Mental Health, Infant and Maternal Mortality as well as various other medical specialty updates, research, and Medical Jeopardy.” The second part of the morning session was on Diabetes and Kidney Disease. The scientific presentation on Diabetes Management Update was given by Dr. G.R. Sridhar, while “Diabetic Nephropathy: Current Concepts in Diagnosis” was offered by Dr. Sharma Prabhakar. Dr. K. L. Gupta educated the audience on Lupus Nephritis. “CKD of Unknown Origin & Uddanam Nephropathy” was the theme addressed by Dr. T. Ravi Raju, while “New Insights into the Biology and Mechanism of Renal Fibrosis” was the topic addressed by Dr. Raghu Kalluri. The sessions were moderated by Dr. KAV Subrahmanyam, Dr. K. Dilip Kumar, and Dr. R. K. Sharma.
The second part of the morning session was on Diabetes and Kidney Disease. The scientific presentation on Diabetes Management Update was given by Dr. G.R. Sridhar, while “Diabetic Nephropathy: Current Concepts in Diagnosis” was offered by Dr. Sharma Prabhakar. Dr. K. L. Gupta educated the audience on Lupus Nephritis. “CKD of Unknown Origin & Uddanam Nephropathy” was the theme addressed by Dr. T. Ravi Raju, while “New Insights into the Biology and Mechanism of Renal Fibrosis” was the topic addressed by Dr. Raghu Kalluri. The sessions were moderated by Dr. KAV Subrahmanyam, Dr. K. Dilip Kumar, and Dr. R. K. Sharma. N K Panigrahi opened the session with a brilliant talk on Heart Disease Epidemic, which was followed by an informative session on Heart Failure- What’s New for 2022, presented by Dr. Sreeni Gangasani. Dr. A. Sharath Reddy spoke on Interventional Cardiology Update, and Dr. Brahma Sharma educated the delegates on Current Concepts in Prediction and Prevention of Heart Attacks in South Asians. Structural Heart Disease was the theme of the presentation by Dr. Prasad Chalasani, while Update on Cardiac Surgery was presented by Dr. M. Gopichand.
N K Panigrahi opened the session with a brilliant talk on Heart Disease Epidemic, which was followed by an informative session on Heart Failure- What’s New for 2022, presented by Dr. Sreeni Gangasani. Dr. A. Sharath Reddy spoke on Interventional Cardiology Update, and Dr. Brahma Sharma educated the delegates on Current Concepts in Prediction and Prevention of Heart Attacks in South Asians. Structural Heart Disease was the theme of the presentation by Dr. Prasad Chalasani, while Update on Cardiac Surgery was presented by Dr. M. Gopichand. NATCO Pharma Oncology Session on Sunday, January 8th was chaired by Dr. Satheesh Kathula, Vice President of AAPI, and moderated by Dr. Muralikrishna Voonna and Dr. Sushil Jain. “A focus on newer treatment modalities in Radiation Oncology” was the topic addressed by Dr. Umesh Mahantshetty, while Dr. T. Subramanyeswar Rao spoke about “What’s new in surgical oncology?” An Update on Systemic Therapies for Cancer was provided by Dr. Raghunadharao Digumarti. “Evolving Biology and New Therapies – Strategies to Control Cancer” was the topic addressed by Dr. Raghu Kalluri. An insightful session on Pharmaco economics of cancer drugs – can we afford it?” was presented by Dr. Satheesh Kathula. “India’s unique value proposition towards Medical Tourism” was addressed by Mr. Shaaz Mehmood.
NATCO Pharma Oncology Session on Sunday, January 8th was chaired by Dr. Satheesh Kathula, Vice President of AAPI, and moderated by Dr. Muralikrishna Voonna and Dr. Sushil Jain. “A focus on newer treatment modalities in Radiation Oncology” was the topic addressed by Dr. Umesh Mahantshetty, while Dr. T. Subramanyeswar Rao spoke about “What’s new in surgical oncology?” An Update on Systemic Therapies for Cancer was provided by Dr. Raghunadharao Digumarti. “Evolving Biology and New Therapies – Strategies to Control Cancer” was the topic addressed by Dr. Raghu Kalluri. An insightful session on Pharmaco economics of cancer drugs – can we afford it?” was presented by Dr. Satheesh Kathula. “India’s unique value proposition towards Medical Tourism” was addressed by Mr. Shaaz Mehmood. The much-anticipated Women’s Leadership Forum featured extraordinarily successful Women Leaders representing a diversity of professions, involving public, private and government organizations.
The much-anticipated Women’s Leadership Forum featured extraordinarily successful Women Leaders representing a diversity of professions, involving public, private and government organizations. Medical Education & Research was led by Dr. Lokesh Eadara, Dr. P.V. Sudhakar, and Dr. G. Butchiraju. Community Outreach Program – HPV Vaccination at the Mahatma Gandhi Cancer Hospital, Visakhapatnam was coordinated by Dr. Syed Ahmed, Dr. Murali Krishna Voona, Dr. Meher Bala Medavaram, Secretary of AAPI.
Medical Education & Research was led by Dr. Lokesh Eadara, Dr. P.V. Sudhakar, and Dr. G. Butchiraju. Community Outreach Program – HPV Vaccination at the Mahatma Gandhi Cancer Hospital, Visakhapatnam was coordinated by Dr. Syed Ahmed, Dr. Murali Krishna Voona, Dr. Meher Bala Medavaram, Secretary of AAPI.
 Dr Ravi Kolli, President of AAPI, while describing the objectives of the Summit, said, “The Global Healthcare Summit has served as a means to raising awareness on key health care issues affecting the Indian subcontinent, such as the Stigma of Mental illness, Suicide prevention, Diabetes, Cardiovascular Diseases, Women’s and Children’s Health, Blindness Prevention and Hepatitis etc. Highlight of this Summit was to reaffirm NRI Physicians’ commitment towards improving health care and create model programs for management of various diseases and to improve outcomes universally, he added.
Dr Ravi Kolli, President of AAPI, while describing the objectives of the Summit, said, “The Global Healthcare Summit has served as a means to raising awareness on key health care issues affecting the Indian subcontinent, such as the Stigma of Mental illness, Suicide prevention, Diabetes, Cardiovascular Diseases, Women’s and Children’s Health, Blindness Prevention and Hepatitis etc. Highlight of this Summit was to reaffirm NRI Physicians’ commitment towards improving health care and create model programs for management of various diseases and to improve outcomes universally, he added. In addition, AAPI has plans to collaborate with various state and federal government programs to enhance the quality of healthcare delivery, making it affordable, efficient, and equitable, improving health outcomes universally and training the trainer sessions involving learning modules in different specialties, and tele-consultations.
In addition, AAPI has plans to collaborate with various state and federal government programs to enhance the quality of healthcare delivery, making it affordable, efficient, and equitable, improving health outcomes universally and training the trainer sessions involving learning modules in different specialties, and tele-consultations. Chief Guest at the Summit, Smt. Vidadala Rajini, Honorable Minister for Health, Family Welfare & Medical Education of state of Andhra Pradesh, said, “The Global Healthcare Summit is an important opportunity for all the healthcare professionals to learn from each other and enhance fellowship. I’m grateful to have this opportunity to attend and learn from all of you,” she said. “I believe that by working with you, we can improve the health and wellbeing of the people in the state. The government has the ability to design the best policies on healthcare, while delivering the best treatments and medical care to the patient is essentially in the hands of the physicians.” Among others who addressed the AAPI delegates and joined the felicitation of AAPI delegates and the local organizers of the Summit included, Shri. Gudivada Amarnath, Honorable Minister for IT.
Chief Guest at the Summit, Smt. Vidadala Rajini, Honorable Minister for Health, Family Welfare & Medical Education of state of Andhra Pradesh, said, “The Global Healthcare Summit is an important opportunity for all the healthcare professionals to learn from each other and enhance fellowship. I’m grateful to have this opportunity to attend and learn from all of you,” she said. “I believe that by working with you, we can improve the health and wellbeing of the people in the state. The government has the ability to design the best policies on healthcare, while delivering the best treatments and medical care to the patient is essentially in the hands of the physicians.” Among others who addressed the AAPI delegates and joined the felicitation of AAPI delegates and the local organizers of the Summit included, Shri. Gudivada Amarnath, Honorable Minister for IT. Describing some of the objectives of the GHS, Dr. Prasad Chalasani, Chair of GHS (USA) 2023 said. “We have tried to create an intellectually charged platform for experts to share their knowledge and experiences on some of the common professional issues that remain a challenge in spite of all the advances. The exchange of expertise and transfer of technology by the best brains is bound to offer positive and innovative solutions to some of the problems faced by humankind.”
Describing some of the objectives of the GHS, Dr. Prasad Chalasani, Chair of GHS (USA) 2023 said. “We have tried to create an intellectually charged platform for experts to share their knowledge and experiences on some of the common professional issues that remain a challenge in spite of all the advances. The exchange of expertise and transfer of technology by the best brains is bound to offer positive and innovative solutions to some of the problems faced by humankind.” AAPI, in collaboration with the AAPI India Foundation administered free HPV vaccines to over 100 low income young women from several government schools in the region, during a special launch and awareness camp organized at the Mahatma Gandhi Cancer Hospital, Visakhapatnam in India on Saturday, January 7th, 2023 with the objective of creating awareness and preventing cervical cancer, a leading cause of cancer deaths among women in India.
AAPI, in collaboration with the AAPI India Foundation administered free HPV vaccines to over 100 low income young women from several government schools in the region, during a special launch and awareness camp organized at the Mahatma Gandhi Cancer Hospital, Visakhapatnam in India on Saturday, January 7th, 2023 with the objective of creating awareness and preventing cervical cancer, a leading cause of cancer deaths among women in India. Dr. Udaya Shivangi, Chair of AAPI’s Women’s Committee, in her opening remarks provided an overview of the Forum and the many initiatives by the Forum both in India and the United States. Shri. MVV Satyavathi, Member of Parliament, representing Anakapalli was the Guest of Honor at the Women’s Forum. In her address, she congratulated AAPI, whose members having been born and educated in India, settled down in the US with success, have come back to India to serve the people of India and work together for the betterment of humanity.
Dr. Udaya Shivangi, Chair of AAPI’s Women’s Committee, in her opening remarks provided an overview of the Forum and the many initiatives by the Forum both in India and the United States. Shri. MVV Satyavathi, Member of Parliament, representing Anakapalli was the Guest of Honor at the Women’s Forum. In her address, she congratulated AAPI, whose members having been born and educated in India, settled down in the US with success, have come back to India to serve the people of India and work together for the betterment of humanity. The women leaders of AAPI dazzled on stage with elegance, and showcasing their talents by presenting two amazing Fashion Shows on Friday and Saturday at the Summit to the delight of the AAPI delegates.
The women leaders of AAPI dazzled on stage with elegance, and showcasing their talents by presenting two amazing Fashion Shows on Friday and Saturday at the Summit to the delight of the AAPI delegates.



































 All women experience menopause differently, and many women experience changes in their sex life as they go through menopause. The loss of estrogen and testosterone following menopause induces multiple changes in a woman’s body and influences sexual function. Also, lower levels of estrogen can cause a drop in blood supply to the vagina, which can affect vaginal lubrication, causing the vagina to be too dry for comfortable sex. Moreover, other menopausal symptoms like bladder control problems, sleep disturbances, depression or anxiety, stress, medications, and other health concerns also affect the sexual well-being of the women experiencing menopause.
All women experience menopause differently, and many women experience changes in their sex life as they go through menopause. The loss of estrogen and testosterone following menopause induces multiple changes in a woman’s body and influences sexual function. Also, lower levels of estrogen can cause a drop in blood supply to the vagina, which can affect vaginal lubrication, causing the vagina to be too dry for comfortable sex. Moreover, other menopausal symptoms like bladder control problems, sleep disturbances, depression or anxiety, stress, medications, and other health concerns also affect the sexual well-being of the women experiencing menopause. The gala began with Dr. Uma Johnnalagadda, President of GAPI, Dr. Sreeni Ganagasani, and Dr. Raghu Lolabhattu, welcoming community members, family, friends, colleagues, and sponsors. “We, the AAPI-GAPI team worked hard to stick to the mission of AAPI, for education and charity to serve humanity. We thank each and every member that attended and supported the event. Our special thanks to all our Sponsors,” Dr. Jonnalagadda said.
The gala began with Dr. Uma Johnnalagadda, President of GAPI, Dr. Sreeni Ganagasani, and Dr. Raghu Lolabhattu, welcoming community members, family, friends, colleagues, and sponsors. “We, the AAPI-GAPI team worked hard to stick to the mission of AAPI, for education and charity to serve humanity. We thank each and every member that attended and supported the event. Our special thanks to all our Sponsors,” Dr. Jonnalagadda said. 
 In his remarks, Dr. Ravi Kolli, President of AAPI, said,” In the context of World Heart Day on September 29th, today’s conference is being organized to educate and create awareness about the major health issue faced by South Asians and offer ways to mitigate heart disease. Dr. Kolli said, “Today’s CME is focused on Recent Advances in South Asian Heart Disease by 2 eminent Indian American physicians who are in the forefront of research and treatment of this deadly disease. It is forward-looking information focusing on cutting edge technologies that can alter the treatment from chronic care model to once and done type of innovative therapies and latest recommendation for actively screening and offering early preventive care to treat cardiovascular disease, especially among the South Asians.”
In his remarks, Dr. Ravi Kolli, President of AAPI, said,” In the context of World Heart Day on September 29th, today’s conference is being organized to educate and create awareness about the major health issue faced by South Asians and offer ways to mitigate heart disease. Dr. Kolli said, “Today’s CME is focused on Recent Advances in South Asian Heart Disease by 2 eminent Indian American physicians who are in the forefront of research and treatment of this deadly disease. It is forward-looking information focusing on cutting edge technologies that can alter the treatment from chronic care model to once and done type of innovative therapies and latest recommendation for actively screening and offering early preventive care to treat cardiovascular disease, especially among the South Asians.”  Dr. Jaideep Patel is a cardiologist in Baltimore, Maryland and is affiliated with multiple hospitals in the area, including at the Heart & Vascular Center at Johns Hopkins University, with primary focus on Preventive Cardiology, pointed out that usual risk scoring has been done on Caucasians and cannot be extrapolated to south Asians. Citing Multiethnic Study of Atherosclerosis, that he was part of Dr. Patel said,
Dr. Jaideep Patel is a cardiologist in Baltimore, Maryland and is affiliated with multiple hospitals in the area, including at the Heart & Vascular Center at Johns Hopkins University, with primary focus on Preventive Cardiology, pointed out that usual risk scoring has been done on Caucasians and cannot be extrapolated to south Asians. Citing Multiethnic Study of Atherosclerosis, that he was part of Dr. Patel said,  The new study, published Friday (Sept. 30) in the journal
The new study, published Friday (Sept. 30) in the journal 


 In a letter addressed to the President of the General Assembly, E. Courtenay Rattray Chef de Cabinet, says “while there is strong support for the return to a pre-pandemic General Debate, as reflected by the level of inscriptions by Member States in the provisional list of speakers– and an improvement in the environment as compared to the last two years– we also recognize that we are not free from the Coronavirus and its impact.”
In a letter addressed to the President of the General Assembly, E. Courtenay Rattray Chef de Cabinet, says “while there is strong support for the return to a pre-pandemic General Debate, as reflected by the level of inscriptions by Member States in the provisional list of speakers– and an improvement in the environment as compared to the last two years– we also recognize that we are not free from the Coronavirus and its impact.” The first of a kind program administered free HPV vaccines to the poor and underserved adolescent girls at the local Tanvir Hospital in Srinagar Colony, Hyderabad in India with the objective of preventing HPV related cancers, including cervical cancer, which is a leading cause of cancer deaths among women in India. The initial launch of the program was held on January 9
The first of a kind program administered free HPV vaccines to the poor and underserved adolescent girls at the local Tanvir Hospital in Srinagar Colony, Hyderabad in India with the objective of preventing HPV related cancers, including cervical cancer, which is a leading cause of cancer deaths among women in India. The initial launch of the program was held on January 9 Usually, cervical cancer develops slowly over time, and another powerful preventive measure is Pap test
Usually, cervical cancer develops slowly over time, and another powerful preventive measure is Pap test Called Vuity, the drop is applied to each eye once a day and starts working within 15 minutes of application. The makers say each drop lasts for at least six hours. As per the report, the drug is a formulation of a well-known compound known as pilocarpine.
Called Vuity, the drop is applied to each eye once a day and starts working within 15 minutes of application. The makers say each drop lasts for at least six hours. As per the report, the drug is a formulation of a well-known compound known as pilocarpine. India celebrated its dedication commitment to prevent Covid virus as it has now provided over two billion Billion Vaccines to its 1.4 billion people. Celebrations were across the nation, after India administered 2 billion doses of vaccinations against COVID-19.
India celebrated its dedication commitment to prevent Covid virus as it has now provided over two billion Billion Vaccines to its 1.4 billion people. Celebrations were across the nation, after India administered 2 billion doses of vaccinations against COVID-19.  As an Indian American growing up in Miami, he was an excellent student, but he worried about not having anyone to sit next to in the cafeteria. The food in his lunch bag was different from what the other kids had. His skin tone was different. His parents were different. “When you’re really shy and when your self-esteem is as low as it was for me as a child,” he says, “I knew those differences made me feel like I didn’t belong.”
As an Indian American growing up in Miami, he was an excellent student, but he worried about not having anyone to sit next to in the cafeteria. The food in his lunch bag was different from what the other kids had. His skin tone was different. His parents were different. “When you’re really shy and when your self-esteem is as low as it was for me as a child,” he says, “I knew those differences made me feel like I didn’t belong.” At least at first,
At least at first, 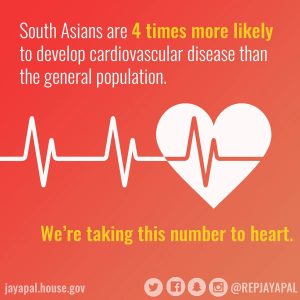 Heart disease is the number one Global Public Health problem. South Asians are at a four-times greater risk of heart disease than their western counterparts and have a greater chance of having a heart attack before 50 years of age, says a . Heart attacks strike South Asian Men and Women at younger ages, and as a result, both morbidity and mortality are higher among them compared to any other ethnic group. They tend to develop heart disease ten years earlier than other groups.”
Heart disease is the number one Global Public Health problem. South Asians are at a four-times greater risk of heart disease than their western counterparts and have a greater chance of having a heart attack before 50 years of age, says a . Heart attacks strike South Asian Men and Women at younger ages, and as a result, both morbidity and mortality are higher among them compared to any other ethnic group. They tend to develop heart disease ten years earlier than other groups.”  In his keynote address, Ambassador Taranjit Singh Sandhu lauded the several initiatves of AAPI over the past four decades and said, “Over the past four decades, AAPI has been doing an outstanding job in advocacy and health education. You play an important role, especially during the Covid Pandemic/” Speaking at length on the growing Indo-US relationship, the veteran diplomat said, “Over the last two decades, India and the United States have overcome the hesitations of history and fashioned a remarkable partnership, built on a bipartisan consensus in the U.S. and cross-party support in India.” Elaborating on the collaboration between India and the US, he said, “From the provision of active pharmaceutical ingredients to generic medicines that have lowered drug prices and created jobs and investments, India has demonstrated its reliability as a supply chain partner, especially as de-risking from single country supplies has become a priority.”
In his keynote address, Ambassador Taranjit Singh Sandhu lauded the several initiatves of AAPI over the past four decades and said, “Over the past four decades, AAPI has been doing an outstanding job in advocacy and health education. You play an important role, especially during the Covid Pandemic/” Speaking at length on the growing Indo-US relationship, the veteran diplomat said, “Over the last two decades, India and the United States have overcome the hesitations of history and fashioned a remarkable partnership, built on a bipartisan consensus in the U.S. and cross-party support in India.” Elaborating on the collaboration between India and the US, he said, “From the provision of active pharmaceutical ingredients to generic medicines that have lowered drug prices and created jobs and investments, India has demonstrated its reliability as a supply chain partner, especially as de-risking from single country supplies has become a priority.”
 Dr. Anjana Sammadar, President-Elect , pointed out: “There was a sense of joy and relief on the faces of the over 1,000 physicians who have come together to celebrate their achievements, contributions, and to network and deepen their relationship even as the Covid Pandemic is waning and people are able to mingle freely and interact with one another cautiously.”
Dr. Anjana Sammadar, President-Elect , pointed out: “There was a sense of joy and relief on the faces of the over 1,000 physicians who have come together to celebrate their achievements, contributions, and to network and deepen their relationship even as the Covid Pandemic is waning and people are able to mingle freely and interact with one another cautiously.” 

 Dr. Jagan Ailinani was honored with Life Time Achievement Award. The Distinguished Physician Award was given to Dr. Vijay Yeldandi and AAPI’s Most Distinguished Award was given to Dr. Ravindra Nathan. AAPI’s Most Distinguished YPS Award was given to Dr. Sejal Hathi and the AAPI’s Most Distinguished MSRF Award was given to Aaiswariya Gulani. r. Gotimukula honored Dr. Udaya Shivangi, Dr. Sujeeth Punnam, Dr. Dwarkanath Reddy and AAPI’s Legal Advisor with Presidential Awards for their dedication and support during her presidency.
Dr. Jagan Ailinani was honored with Life Time Achievement Award. The Distinguished Physician Award was given to Dr. Vijay Yeldandi and AAPI’s Most Distinguished Award was given to Dr. Ravindra Nathan. AAPI’s Most Distinguished YPS Award was given to Dr. Sejal Hathi and the AAPI’s Most Distinguished MSRF Award was given to Aaiswariya Gulani. r. Gotimukula honored Dr. Udaya Shivangi, Dr. Sujeeth Punnam, Dr. Dwarkanath Reddy and AAPI’s Legal Advisor with Presidential Awards for their dedication and support during her presidency. Dr. Anupama Gotimukula, the Immediate Past President of AAPI said, “Our leadership team has worked diligently on so many wonderful projects and activities including educational, philanthropic, legislative, networking, and many more activities benefitting our members and communities. This has been possible because of the incredible work and support from the dedicated team of leaders, members, and our supporting office staff,” the only 4th woman President of AAPI in the four decades long history of AAPI, said.
Dr. Anupama Gotimukula, the Immediate Past President of AAPI said, “Our leadership team has worked diligently on so many wonderful projects and activities including educational, philanthropic, legislative, networking, and many more activities benefitting our members and communities. This has been possible because of the incredible work and support from the dedicated team of leaders, members, and our supporting office staff,” the only 4th woman President of AAPI in the four decades long history of AAPI, said. Dr. V. Ranga in his address he said, “My goal in the coming year is to formalize and create AAPI leadership academy working with executives from American College of Physicians for the development of leadership roles for all AAPI members. I want to work hard to engage young physicians and attract them to AAPI. They are the future of AAPI.”
Dr. V. Ranga in his address he said, “My goal in the coming year is to formalize and create AAPI leadership academy working with executives from American College of Physicians for the development of leadership roles for all AAPI members. I want to work hard to engage young physicians and attract them to AAPI. They are the future of AAPI.” In his keynote address, Ambassador Taranjit Singh Sandhu lauded the several initiatves of AAPI over the past four decades and said, “Over the past four decades, AAPI has been doing an outstanding job in advocacy and health education. You play an important role, especially during the Covid Pandemic/” Speaking at length on the growing Indo-US relationship, the veteran diplomat said, “Over the last two decades, India and the United States have overcome the hesitations of history and fashioned a remarkable partnership, built on a bipartisan consensus in the U.S. and cross-party support in India.” Elaborating on the collaboration between India and the US, he said, “From the provision of active pharmaceutical ingredients to generic medicines that have lowered drug prices and created jobs and investments, India has demonstrated its reliability as a supply chain partner, especially as de-risking from single country supplies has become a priority.”
In his keynote address, Ambassador Taranjit Singh Sandhu lauded the several initiatves of AAPI over the past four decades and said, “Over the past four decades, AAPI has been doing an outstanding job in advocacy and health education. You play an important role, especially during the Covid Pandemic/” Speaking at length on the growing Indo-US relationship, the veteran diplomat said, “Over the last two decades, India and the United States have overcome the hesitations of history and fashioned a remarkable partnership, built on a bipartisan consensus in the U.S. and cross-party support in India.” Elaborating on the collaboration between India and the US, he said, “From the provision of active pharmaceutical ingredients to generic medicines that have lowered drug prices and created jobs and investments, India has demonstrated its reliability as a supply chain partner, especially as de-risking from single country supplies has become a priority.” Dozens of local children from ages 8 to 16, trained by Yoga Masters in San Antonio by presenting and demonstrating multiple Yoga Aasanas to the tune of Vande Mataram provided valuable education on Yoga and its importance in life. Every evening the popular AAPI Got Talent and
Dozens of local children from ages 8 to 16, trained by Yoga Masters in San Antonio by presenting and demonstrating multiple Yoga Aasanas to the tune of Vande Mataram provided valuable education on Yoga and its importance in life. Every evening the popular AAPI Got Talent and Describing it to be a “historic 40th annual convention celebrating 40 years of AAPI and India’s 75 years of Independence in collaboration with the Indian Consulate in Houston and Indian Embassy with invited dignitaries from the US and India,” Dr. Anupama Gotimukula, the only 4th woman President of AAPI in the four decades-long history of AAP, expressed gratitude to “the entire AAPI leadership and members for their participation in AAPI activities, making AAPI stronger.”
Describing it to be a “historic 40th annual convention celebrating 40 years of AAPI and India’s 75 years of Independence in collaboration with the Indian Consulate in Houston and Indian Embassy with invited dignitaries from the US and India,” Dr. Anupama Gotimukula, the only 4th woman President of AAPI in the four decades-long history of AAP, expressed gratitude to “the entire AAPI leadership and members for their participation in AAPI activities, making AAPI stronger.” Welcoming AAPI delegates to San Antonio, Ron Nirenberg, Mayor of San Antonio, whom Dr. Jayesh Shah called as the next Governor of Texas, declared June 24th as AAPI Day and International Yoga Day in the City of San Antonio. While praising AAPI and its members for their contributions, Nirenberg said, “We are honored to host the largest gathering of Indian American physicians in our vibrant city, home to some of the best healthcare facilities in the nation.”
Welcoming AAPI delegates to San Antonio, Ron Nirenberg, Mayor of San Antonio, whom Dr. Jayesh Shah called as the next Governor of Texas, declared June 24th as AAPI Day and International Yoga Day in the City of San Antonio. While praising AAPI and its members for their contributions, Nirenberg said, “We are honored to host the largest gathering of Indian American physicians in our vibrant city, home to some of the best healthcare facilities in the nation.” By encouraging manufacturing, innovation, and R&D based on emerging technological landscapes, and transforming India into a hub for medical devices, India may emerge as the “diagnostic capital of the world,” Mahajan said.
By encouraging manufacturing, innovation, and R&D based on emerging technological landscapes, and transforming India into a hub for medical devices, India may emerge as the “diagnostic capital of the world,” Mahajan said. Gavaskar said, he had wanted to be a Doctor as a youth, after he was a witness to how his aunt, a Doctor by profession had touched so many lives by the care she had provided. “Yours is the greatest of all professions in the world. You have put your lives at risk during the Pandemic to save the lives of others. Yours is the noble profession that I have admired always.”
Gavaskar said, he had wanted to be a Doctor as a youth, after he was a witness to how his aunt, a Doctor by profession had touched so many lives by the care she had provided. “Yours is the greatest of all professions in the world. You have put your lives at risk during the Pandemic to save the lives of others. Yours is the noble profession that I have admired always.” In her spiritual discourse, Sadhvi Bhagawati Saraswati, PhD, Spiritual leader, teacher and author, said, “It’s such a joy to be here. Such a deep gratitude. Covid did not create you as heroes, but you have been heroes all along.” Sharing her own personal journey, she said, we all have only one life and how her coming to the banks of the Himalayas, transformed her own lifafter having experienced the unique culture and wisdom of India. While pointing to how we are creating a vicious negative health through fear, stress and anxiety in this country, her message today was to focus on the Synonym for HEALTH: Health, Embrace, Allow, Love, Time for yourself, and Help others.
In her spiritual discourse, Sadhvi Bhagawati Saraswati, PhD, Spiritual leader, teacher and author, said, “It’s such a joy to be here. Such a deep gratitude. Covid did not create you as heroes, but you have been heroes all along.” Sharing her own personal journey, she said, we all have only one life and how her coming to the banks of the Himalayas, transformed her own lifafter having experienced the unique culture and wisdom of India. While pointing to how we are creating a vicious negative health through fear, stress and anxiety in this country, her message today was to focus on the Synonym for HEALTH: Health, Embrace, Allow, Love, Time for yourself, and Help others. In his live video message, Paramaguru Sharath Jois, Lineage holder of Ashtanga Yoga, told AAPI leaders as to how “each of you have sacrificed your life. I congratulate the organizers for focusing on heal the healers and using Yoga our traditional method to help us in our daily lives.” In his message, he said, “We all experience similar things in life, but respond from our inner self. How we tend to react to people and situations makes the difference. When you abuse a situation it’s agitation, but when you use them effectively it’s liberation.” Referring to the 7th anniversary of India’s Independence he said, “It must help us transcend all that divide us on the basis of caste, creed and status.”
In his live video message, Paramaguru Sharath Jois, Lineage holder of Ashtanga Yoga, told AAPI leaders as to how “each of you have sacrificed your life. I congratulate the organizers for focusing on heal the healers and using Yoga our traditional method to help us in our daily lives.” In his message, he said, “We all experience similar things in life, but respond from our inner self. How we tend to react to people and situations makes the difference. When you abuse a situation it’s agitation, but when you use them effectively it’s liberation.” Referring to the 7th anniversary of India’s Independence he said, “It must help us transcend all that divide us on the basis of caste, creed and status.” The panelists at the prestigious Women’s Forum included: Dr. Juby A. Jacob-Nara, a Public Health Physician, Vice President and Head of Global Medical Respiratory Allergy & Gastroenterology (Sanofi-Genzyme) who has been a part of over 50 new medicines successfully launched including vaccines in the US and globally; Dr. Kalpalatha Guntupalli, Endowed Professor for Pulmonary Disorders, Baylor College of Medicine; Dr. Sowjanya Mohan, Group Chief Medical Officer, Texas Group/Tenet Health; and, Ms. Rosemary Hickman, Semmes Foundation Education Manager at the Mcnay Art Museum.
The panelists at the prestigious Women’s Forum included: Dr. Juby A. Jacob-Nara, a Public Health Physician, Vice President and Head of Global Medical Respiratory Allergy & Gastroenterology (Sanofi-Genzyme) who has been a part of over 50 new medicines successfully launched including vaccines in the US and globally; Dr. Kalpalatha Guntupalli, Endowed Professor for Pulmonary Disorders, Baylor College of Medicine; Dr. Sowjanya Mohan, Group Chief Medical Officer, Texas Group/Tenet Health; and, Ms. Rosemary Hickman, Semmes Foundation Education Manager at the Mcnay Art Museum. Some of the major themes at the convention include: Yoga and Meditation practices, Welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, Ailment based yoga therapy sessions, Workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine. Yoga gurus and experts leading the wellness sessions include Paramguru Sharatha Jois, Sadhvi Bhagawati, Saraswati Eddie Stern, Dr. Sat Bir Khalsa, Dr. Dilip Sarkar, Dr. Pankaj Vij, and Dr. Param Dedhia.
Some of the major themes at the convention include: Yoga and Meditation practices, Welcome kit with books & self-care supplies, A Personal Reflexology Session, Take home wellness routine, Ailment based yoga therapy sessions, Workshop on Spiritual well-being, Book talk with Yoga Gurus, including on the science of Yoga & Lifestyle medicine. Yoga gurus and experts leading the wellness sessions include Paramguru Sharatha Jois, Sadhvi Bhagawati, Saraswati Eddie Stern, Dr. Sat Bir Khalsa, Dr. Dilip Sarkar, Dr. Pankaj Vij, and Dr. Param Dedhia. AAPI delegates have the opportunity to attend a multidisciplinary CME conference that allows specialists and primary care physicians to interact in an academic forum. World-renowned speakers discussed gaps between current and best practice of wide-ranging topics at the CME sessions.
AAPI delegates have the opportunity to attend a multidisciplinary CME conference that allows specialists and primary care physicians to interact in an academic forum. World-renowned speakers discussed gaps between current and best practice of wide-ranging topics at the CME sessions. Dr. Kolli understands the importance of assuming charge as the President of AAPI, “a very prestigious, dedicated, and powerful organization, representing over 120,000 physicians of Indian origin, with an active membership of at least 14,000 life members and in addition to the members of the more than 120 local chapters, chapters of Alumni and Specialty associations across the nation. Being a leader of this organization is a great honor and responsibility,” Dr. Kolli says, “With great power comes to a greater responsibility as well” and believes that “To whomever much is given, of him will much be required; and to whom much was entrusted, of him more will be asked.”
Dr. Kolli understands the importance of assuming charge as the President of AAPI, “a very prestigious, dedicated, and powerful organization, representing over 120,000 physicians of Indian origin, with an active membership of at least 14,000 life members and in addition to the members of the more than 120 local chapters, chapters of Alumni and Specialty associations across the nation. Being a leader of this organization is a great honor and responsibility,” Dr. Kolli says, “With great power comes to a greater responsibility as well” and believes that “To whomever much is given, of him will much be required; and to whom much was entrusted, of him more will be asked.” Empowering physicians as the leaders in the delivery of evidence-based health care by engaging with policymakers, governmental agencies at all levels and the private sector is a major area where Dr. Kolli wants to direct the efforts for AAPI. Some of the other areas, he wants AAPI to focus on under his leadership include: Connect with the next generation physicians for their participation in all areas of organizational leadership and activities; Advocate for expediting the GC Backlog for physicians through legislation; Promotion of mental health awareness, tackling mental illness, substance abuse and suicide devastating the nation; Planning International Medical Missions with our AAPI physicians to serve communities globally.
Empowering physicians as the leaders in the delivery of evidence-based health care by engaging with policymakers, governmental agencies at all levels and the private sector is a major area where Dr. Kolli wants to direct the efforts for AAPI. Some of the other areas, he wants AAPI to focus on under his leadership include: Connect with the next generation physicians for their participation in all areas of organizational leadership and activities; Advocate for expediting the GC Backlog for physicians through legislation; Promotion of mental health awareness, tackling mental illness, substance abuse and suicide devastating the nation; Planning International Medical Missions with our AAPI physicians to serve communities globally. Growing up in a family where his dad was a state government official in the Andhra Pradesh state transportation department, Dr. Kolli and his family traveled from place to place every three years with the transfer of his dad, which was a huge challenge. However, “That gave me a wider and unique perspective on life, with the opportunity to meet new people, in new places and environments. It was an enriching experience in some ways and though we didn’t have any roots in one place, we had a wider network of friends and associates all around the state.”
Growing up in a family where his dad was a state government official in the Andhra Pradesh state transportation department, Dr. Kolli and his family traveled from place to place every three years with the transfer of his dad, which was a huge challenge. However, “That gave me a wider and unique perspective on life, with the opportunity to meet new people, in new places and environments. It was an enriching experience in some ways and though we didn’t have any roots in one place, we had a wider network of friends and associates all around the state.”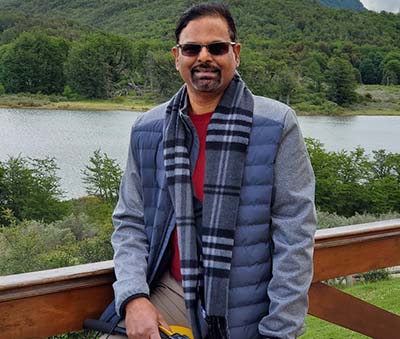 “AAPI is very young, dynamic, and active,” Dr. Kolli says. “Every year nearly 500 -1000 new members are joining AAPI. My goal is to bring as many like-minded people as possible who are loyal and committed to AAPI goals and values, on one page, one theme, and on one track to solve the problems collectively. It is important for us not to stay apart and fall apart but come together and stand together and make AAPI strong.”
“AAPI is very young, dynamic, and active,” Dr. Kolli says. “Every year nearly 500 -1000 new members are joining AAPI. My goal is to bring as many like-minded people as possible who are loyal and committed to AAPI goals and values, on one page, one theme, and on one track to solve the problems collectively. It is important for us not to stay apart and fall apart but come together and stand together and make AAPI strong.” Despite his busy schedule, Dr. Kolli makes time available to play Rummy and socialize with three diverse groups of friends regularly for over a quarter-century. “We have a Kannada group of friends. I have a Telugu group of friends and a group of friends from all over India, from Himachal Pradesh, Punjab, Rajasthan, Gujarat, Maharashtra, Telangana, and Karnataka as well as other regions with whom I play cards on some weekends, which is great opportunity to connect, belong, socialize and relax.”
Despite his busy schedule, Dr. Kolli makes time available to play Rummy and socialize with three diverse groups of friends regularly for over a quarter-century. “We have a Kannada group of friends. I have a Telugu group of friends and a group of friends from all over India, from Himachal Pradesh, Punjab, Rajasthan, Gujarat, Maharashtra, Telangana, and Karnataka as well as other regions with whom I play cards on some weekends, which is great opportunity to connect, belong, socialize and relax.” A major theme during the 40th annual convention is “Physician, heal thyself,” acknowledging and seeking to respond to the growing signs of burnout among physicians, by offering positive remedial resources as part of the first-ever Wellness Program being offered to participants at the 40th annual Convention of AAPI to be held in san Antonio from June 23rd to 26th, 2022 at Henry B Gonzalez Convention Center.
A major theme during the 40th annual convention is “Physician, heal thyself,” acknowledging and seeking to respond to the growing signs of burnout among physicians, by offering positive remedial resources as part of the first-ever Wellness Program being offered to participants at the 40th annual Convention of AAPI to be held in san Antonio from June 23rd to 26th, 2022 at Henry B Gonzalez Convention Center. The Convention will honor India and its 75 years of Independence Day celebrations- co-sponsored by the Embassy of India & the Consulate General of India (CGI) – Houston.
The Convention will honor India and its 75 years of Independence Day celebrations- co-sponsored by the Embassy of India & the Consulate General of India (CGI) – Houston. Envisioned and built against the backdrop of COVID-19 challenges that stretched our health care system to the brink, including increased physician
Envisioned and built against the backdrop of COVID-19 challenges that stretched our health care system to the brink, including increased physician  If yes, this is probably because of your environment and poor pre-sleep discipline. To have the sleep that you are looking for, you need to work hard. Create an environment, which works best for you.
If yes, this is probably because of your environment and poor pre-sleep discipline. To have the sleep that you are looking for, you need to work hard. Create an environment, which works best for you. The authors also note that although firearm fatality rates started to rise in 2014, the dramatic societal upheaval of the COVID-19 pandemic likely accelerated this increase with the escalation of mental health stressors and existential despair experienced by youth. The seismic shift in youths’ lives during the pandemic occurred in the context of a decades’ long void of prevention efforts to decrease firearm injuries and deaths.
The authors also note that although firearm fatality rates started to rise in 2014, the dramatic societal upheaval of the COVID-19 pandemic likely accelerated this increase with the escalation of mental health stressors and existential despair experienced by youth. The seismic shift in youths’ lives during the pandemic occurred in the context of a decades’ long void of prevention efforts to decrease firearm injuries and deaths.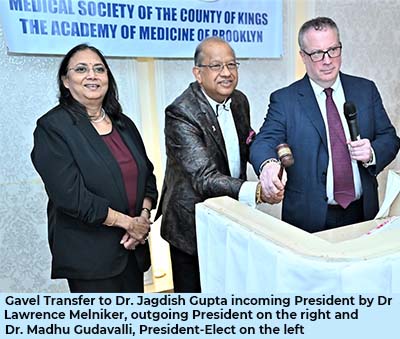 Dr. Gupta was addressing the delegates at the 201st Annual Stated Meeting of MSCK as a Bicentennial Event in person, after two years hiatus due to COVID Pandemic at El Caribe Country Club in Brooklyn, NY with full regalia. “The COVID-19 pandemic upended the rhythms of our personal and professional lives. Traditional workings of our medical society came to a screeching halt,” Dr. Gupta pointed out. “However, as an organization, we persevered, reimagined our operations, and implemented new strategies. Overall, the organization was renewed and brought into the 21st century.”
Dr. Gupta was addressing the delegates at the 201st Annual Stated Meeting of MSCK as a Bicentennial Event in person, after two years hiatus due to COVID Pandemic at El Caribe Country Club in Brooklyn, NY with full regalia. “The COVID-19 pandemic upended the rhythms of our personal and professional lives. Traditional workings of our medical society came to a screeching halt,” Dr. Gupta pointed out. “However, as an organization, we persevered, reimagined our operations, and implemented new strategies. Overall, the organization was renewed and brought into the 21st century.” Dr. Sanjiv Chopra, Professor of Medicine and the past Faculty Dean for Continuing Medical Education at Harvard Medical School for 12 years, serving as a Marshall Wolf Distinguished Clinician Educator at Brigham and Women’s Hospital, and the author of more than 170 publications and ten books to his credit, was the keynote speaker at the gala. In his address, he pointed out to “The Two Most Important Days: Reflections on Lasting Happiness and Living with Purpose.” He received a full-throttled standing ovation from the audience. Dr. Chopra is Editor-in-Chief of the Hepatology Section of “UpToDate”, the most widely used electronic textbook in the world subscribed to by more than 1.5 million physicians in 195 countries.
Dr. Sanjiv Chopra, Professor of Medicine and the past Faculty Dean for Continuing Medical Education at Harvard Medical School for 12 years, serving as a Marshall Wolf Distinguished Clinician Educator at Brigham and Women’s Hospital, and the author of more than 170 publications and ten books to his credit, was the keynote speaker at the gala. In his address, he pointed out to “The Two Most Important Days: Reflections on Lasting Happiness and Living with Purpose.” He received a full-throttled standing ovation from the audience. Dr. Chopra is Editor-in-Chief of the Hepatology Section of “UpToDate”, the most widely used electronic textbook in the world subscribed to by more than 1.5 million physicians in 195 countries. Among the several distinguished guests who joined in and addressed the celebrations were Brooklyn District Attorney Eric Gonzalez who spoke passionately about the need for Gun Control and on ways to prevent the violence in the City. Messages and proclamations were sent in by New York City Council Woman Ms. Mercedes Narcisse 46th Council District; Congresswoman Nicole Malliotakis from 11th District; President of SUNY Downstate Medical School, Dr. Wayne Riley who spoke about the contribution of Medical Society of County of Kings and Long Island College over 200 years; State Assemblyman Michael Tannousis; Dr. Ravi Kolli, President Elect, American Association of Physicians of Indian Origin- the largest ethnic physician organization in America; and, Multiple Citations for 50 years Medical School Graduates serving the Brooklyn Community.
Among the several distinguished guests who joined in and addressed the celebrations were Brooklyn District Attorney Eric Gonzalez who spoke passionately about the need for Gun Control and on ways to prevent the violence in the City. Messages and proclamations were sent in by New York City Council Woman Ms. Mercedes Narcisse 46th Council District; Congresswoman Nicole Malliotakis from 11th District; President of SUNY Downstate Medical School, Dr. Wayne Riley who spoke about the contribution of Medical Society of County of Kings and Long Island College over 200 years; State Assemblyman Michael Tannousis; Dr. Ravi Kolli, President Elect, American Association of Physicians of Indian Origin- the largest ethnic physician organization in America; and, Multiple Citations for 50 years Medical School Graduates serving the Brooklyn Community.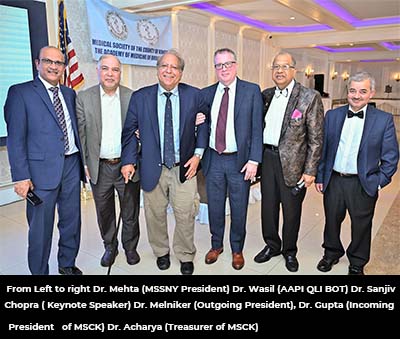 The Medical Society of the County of Kings (MSCK), the oldest scientific organization in Brooklyn, New York was established on March 2nd, 1822 by a group of doctors gathered at Auld Lang Syne Tavern on Fulton Street in Brooklyn Heights, with the lofty mission “to foster progress in the science and art of medicine and to promote, preserve and enforce the highest of standards of ethical and proficient medical care”. In 1900, the Society opened its grand new colonial revival building at 1313 Bedford Avenue, the geographical center of Brooklyn and It was headquartered there until 1996.
The Medical Society of the County of Kings (MSCK), the oldest scientific organization in Brooklyn, New York was established on March 2nd, 1822 by a group of doctors gathered at Auld Lang Syne Tavern on Fulton Street in Brooklyn Heights, with the lofty mission “to foster progress in the science and art of medicine and to promote, preserve and enforce the highest of standards of ethical and proficient medical care”. In 1900, the Society opened its grand new colonial revival building at 1313 Bedford Avenue, the geographical center of Brooklyn and It was headquartered there until 1996. Dr Tedros decides on the awardees for the World Health Organisation Director-General’s Global Health Leaders Awards. The ceremony for the awards, which were established in 2019, was part of the live-streamed high-level opening session of the 75th World Health Assembly.
Dr Tedros decides on the awardees for the World Health Organisation Director-General’s Global Health Leaders Awards. The ceremony for the awards, which were established in 2019, was part of the live-streamed high-level opening session of the 75th World Health Assembly. But Alito also overlooks the actual issue at stake. If Roe were overturned, it would abrogate the religious freedom and individual rights of several minority religious communities, including U.S. Jews, Muslims and Hindus. These communities support abortion rights in some or all cases in numbers equivalent to or much greater than the general public. That support is often rooted in their faith and the ethics of individual choice.
But Alito also overlooks the actual issue at stake. If Roe were overturned, it would abrogate the religious freedom and individual rights of several minority religious communities, including U.S. Jews, Muslims and Hindus. These communities support abortion rights in some or all cases in numbers equivalent to or much greater than the general public. That support is often rooted in their faith and the ethics of individual choice. Put together by a highly talented and dedicated Team of Convention Committee members, the 4 days long event will be filled with programs and activities that cater to the body, mind and soul. The Convention is going to be a unique experience for everyone, he added.
Put together by a highly talented and dedicated Team of Convention Committee members, the 4 days long event will be filled with programs and activities that cater to the body, mind and soul. The Convention is going to be a unique experience for everyone, he added. Saturday Evening will begin with the Presidential Banquet, which will be followed by a live show by Bollywood’s one of the best “Shaan” Night. Sunday, we bid you “Hasta la Vista” with a closing ceremony,” said Dr. Vijay Koli, Advisor to the Convention.
Saturday Evening will begin with the Presidential Banquet, which will be followed by a live show by Bollywood’s one of the best “Shaan” Night. Sunday, we bid you “Hasta la Vista” with a closing ceremony,” said Dr. Vijay Koli, Advisor to the Convention. Shortly after the leak, the team surveyed potential voters again — 300 in all — to see how the news had affected candidate preference. Even before the leak, abortion was an important issue to most voters. The polls showed that abortion had, on average, a 30% weight in respondents’ candidate preference.
Shortly after the leak, the team surveyed potential voters again — 300 in all — to see how the news had affected candidate preference. Even before the leak, abortion was an important issue to most voters. The polls showed that abortion had, on average, a 30% weight in respondents’ candidate preference.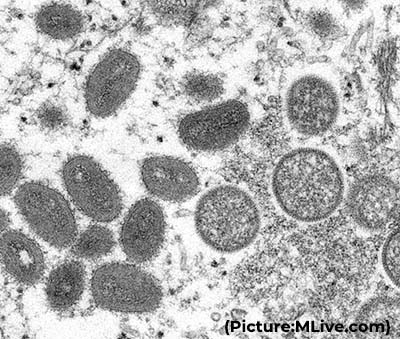 That marks a significant departure from the disease’s typical pattern of spread in central and western Africa, where people are mainly infected by animals like wild rodents and primates and outbreaks have not spread across borders.
That marks a significant departure from the disease’s typical pattern of spread in central and western Africa, where people are mainly infected by animals like wild rodents and primates and outbreaks have not spread across borders. About three-quarters of all Covid-19 deaths have been among seniors, including more than a quarter among people 85 and older, according to CDC data. And while racial and ethnic disparities have lessened over the course of the pandemic, the risk of dying from Covid-19 has been about two times higher for Blacks, Hispanics and American Indians compared to Whites in the US.
About three-quarters of all Covid-19 deaths have been among seniors, including more than a quarter among people 85 and older, according to CDC data. And while racial and ethnic disparities have lessened over the course of the pandemic, the risk of dying from Covid-19 has been about two times higher for Blacks, Hispanics and American Indians compared to Whites in the US. AAPI, the largest ethnic medical organization in the country, representing the interests of over 100,000 physicians of Indian origin, has been focusing on ways to help AAPI members, who have been in the forefront helping millions of patients around the nation, to take care of self and find satisfaction and happiness in the challenging situations they are in, while serving hundreds of patients everyday of their dedicated and noble profession, Dr. Anupama Gotimukula said.
AAPI, the largest ethnic medical organization in the country, representing the interests of over 100,000 physicians of Indian origin, has been focusing on ways to help AAPI members, who have been in the forefront helping millions of patients around the nation, to take care of self and find satisfaction and happiness in the challenging situations they are in, while serving hundreds of patients everyday of their dedicated and noble profession, Dr. Anupama Gotimukula said. “Our practices include heart-based meditation,” said Dr. Chandra Koneru, an Internal Medicine Professional, AAPI member, and Heartfulness Trainer. “Our values align with the American Association of Physicians of Indian Origin (AAPI) mission to facilitate and enable Indian physicians to improve patient care and engage in research that brings distinctive contributions from India.”
“Our practices include heart-based meditation,” said Dr. Chandra Koneru, an Internal Medicine Professional, AAPI member, and Heartfulness Trainer. “Our values align with the American Association of Physicians of Indian Origin (AAPI) mission to facilitate and enable Indian physicians to improve patient care and engage in research that brings distinctive contributions from India.”