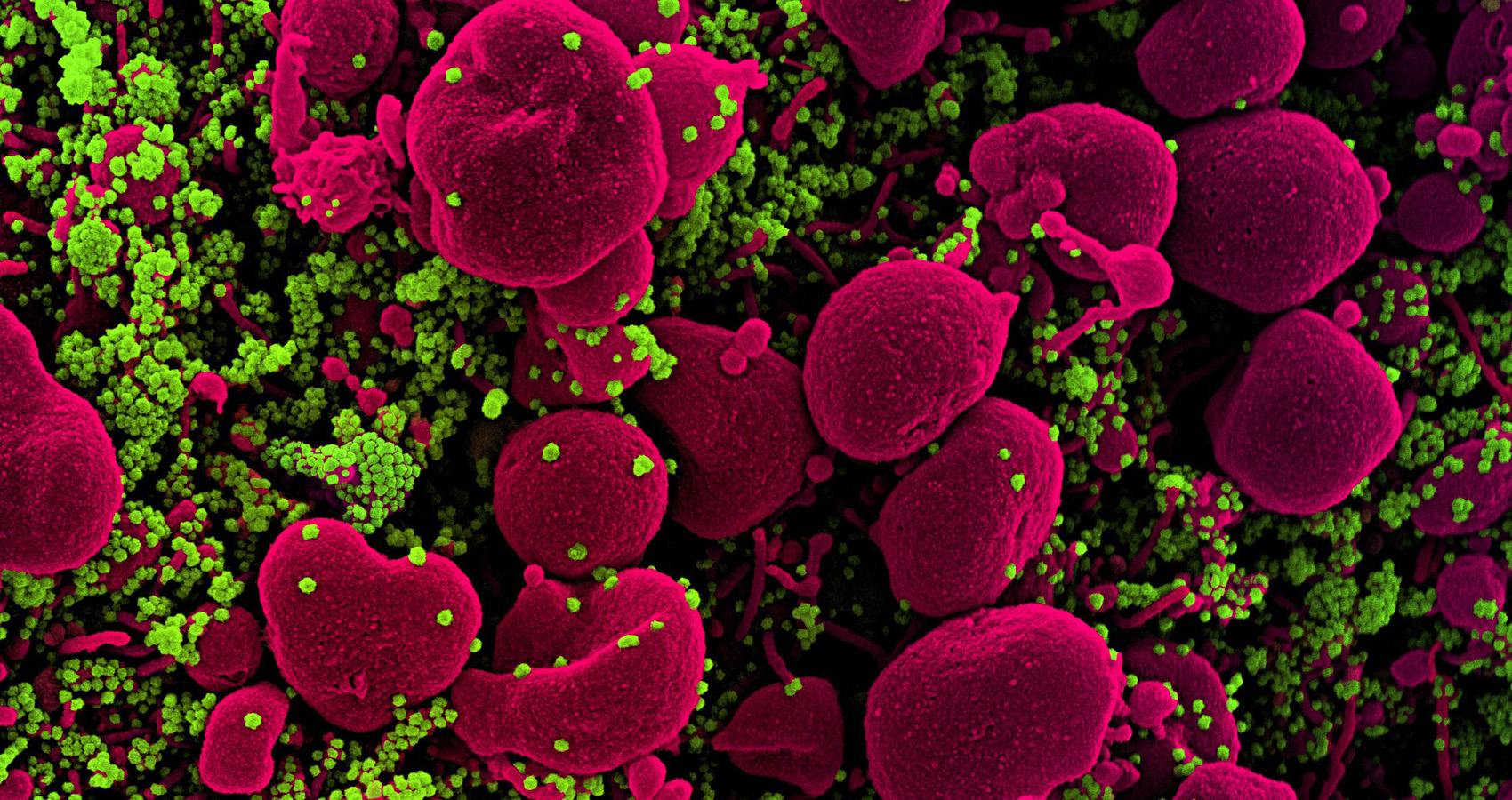
Hooray for COVID Vaccines: An Ounce of Prevention of COVID is Worth a Pound of Cure. Let’s Use That Same Rationale for People Who Already Have COVID.
To be a proponent for early treatment of coronavirus infection shouldn’t automatically mean there is a disregard for the much-needed prevention efforts represented by the mRNA vaccines. This should not be an “either-or” argument. Though there are some who have concerns about the rapid release and production of these novel vaccine interventions, no one can question that we are indeed in a public health crisis and an urgent and expedited effort is what is absolutely warranted (i.e., Operation Warp Speed is actually a fitting name for the rapid response). We get it. However, the broad media coverage on the vaccines seems to obscure any discussion or consideration of formal early treatment interventions for the COVID-positive patient before hospitalization is absolutely required. Early treatment intervention of COVID has the potential to save lives, reduce hospital burden and reduce the need to limit a hospital’s capacity to render other standards of care such as routine surgical interventions.
The death rate of COVID is actually much lower than the actual infection rate, something like only 2% or a little less than 3% maximum. This is a good thing, unless the death rate includes one of your loved ones; then 2% doesn’t seem so negligible. Regardless, complications of COVID can be really challenging for clinicians and downright scary for the rest of the public. It’s been stated at least 10% of COVID survivors develop after effects for up to 6 months or more. Early treatment intervention could potentially reduce the risk of these complications by reducing the progression of COVID to the most serious symptoms and a drastic dash to the local E.D. requiring hospital admission as a minimum, intubation for mechanical ventilation as a maximum.
The reports abound of hospital capacities stretched to their limits and physicians and other clinicians pushed beyond their normal capacities to perform, amidst caring for patients who were originally told to go home and manage on their own, until they have difficulty breathing (of course). Really? This is not the best we can do nor should it be the only consideration.
Let’s take the Ohio State University (OSU) COVID-athlete study into perspective: 26 student athletes who recovered from COVID. Some had symptoms and some actually were asymptomatic (meaning no headache, fever, sniffles or cough, etc.). Myocarditis was observed in 4, or 15%, of these student athletes and in 8, or 30%, the student athletes were observed to have developed cardiac scar tissue. If this is the impact of COVID on young and healthy student athletes (some of whom never developed symptoms), just waiting around until you can’t breathe really shouldn’t be the only outpatient option.
Rather than waiting around for approval from the National Institutes of Health (NIH) or the Centers for Disease Control (CDC), physicians should at least begin to treat the symptoms of COVID in recognition of the over-activation of the inflammatory response is a signal for an advancement of the COVID assault on our bodies. The forecasted intention should be to prevent the COVID-triggered advancement in inflammatory response. So, doctors, what’s the rationale for awaiting a rushed emergency room visit versus a purposeful effort to prevent the mad dash to the E.R. in the first place? Shouldn’t we be activated in preventing this progression of an unchecked inflammatory response (especially since we already know how to keep it from happening)? We must believe in ourselves and standardize an approach to common COVID symptoms using the current medications already in our FDA-indicated/FDA-approved arsenal.
If we were living in a house and heard the alarm sound from the smoke detector, there is no way we would say that there has to be a flame before we take any action (whatsoever). There is no way you would acknowledge that the smoke will transition from a flame to a full-on blaze and only then determine the fire department should be called. Doctor, you would pursue a focused effort to ensure the origin of the smoke was determined and then implement swift action to address whatever caused the smoke in the first place. We would want to make sure the smoke never, ever became a flame and the flame allowed to become the dreaded blaze. Yes, without a doubt, we Early Interventionists are grateful for the new COVID vaccines. The vaccines are a brilliant and valiant effort at a much-needed, long-awaited prevention effort to interrupt the plaque of COVID across our great nation and our world. Nevertheless, these COVID vaccines are not destined for people who already have COVID (at home or in the hospital); the people who are sick at home need prevention too- prevention from hospitalization. Today, as we exhale and celebrate the release of the vaccine to prevent COVID, there are tens of thousands of Americans who are already COVID-positive and not yet hospitalized. By the way, are you wondering about the great mutations?
If You Defend the Body, the Strain Won’t Matter
Treating symptomatic expressions of COVID, before hospital admission, bypasses the need for a specific COVID regimen per se. If your patient has a fever, you address it. If there is evidence of pulmonary dysfunction (like coughing or symptoms of bronchitis, for instance), you would treat it with the standard go-to corticosteroid that you normally would (i.e., prednisone or methylprednisolone). If there is a concern that steroids could further suppress the immune response, then boost the immune system as a precaution. Is anybody concerned that there is now a whole multiple of new COVID strains reported? If we focus on active management of the symptoms (within FDA-indications and -approval, of course) we have a strong likelihood of avoiding the most severe consequences of the infection. Perhaps if we can limit the development of COVID complications in the body, the variations of the strain shouldn’t matter. These efforts are only until the rest of the country has access to the vaccines. However, if essential workers and long-term care, or nursing home, residents are the appropriate priority, there has to be a mitigation plan for treating COVID patients until all who want to be vaccinated can receive the vaccine. Otherwise, are folks to simply try to avoid COVID infection until their vaccine number is called up in April?
We simply must reconsider the intentional plan that says “do nothing until…” it’s a mad panic and rush to the emergency room. The ounce of prevention, to avoid the ambulance, is early treatment intervention of COVID before the infection progresses to the point where hospitalization is required. As staggering as the death toll, the numbers do indeed reflect that more are infected and survive from COVID than those who die from COVID. Nevertheless, there is little comfort in numbers when someone you love and care about is taken from you so tragically and often without any gift of closure in sharing a loving goodbye. Early medicinal intervention in COVID infections as a measure of prevention, against the progression of COVID complications, is critical. Different clinicians have varied approaches towards this end (i.e., Ivermectin, ICAM-similar regimens , etc.) and I have no particular preference. I’m simply grateful they recognize the need to intervene early is undeniable.
Take care of all who want the highly valued prevention effort of the vaccines as soon as possible, but plese don’t forget the folks who already have COVID. Just like the flu vaccines are for people who have not yet contracted the flu, the COVID vaccines are destined for people who have not contracted the COVID infection. Right now, prior to hospitalization, the best effort a COVID patient can obtain is probably thoughts and prayers because their told to ‘go home and come to the E.D. if you get worse or sick or have trouble breathing. However, more and more clinicians have determined that the COVID patient deserves a valiant effort at prevention as well. Let’s not forget, an ounce of prevention could be a great alternative to the need for a COVID ambulance.
(By An Anonymous Healthcare Provider)