In a groundbreaking study published in the journal Cell, a team of scientists has proposed a novel explanation for some cases of long Covid, shedding light on a potential biological pathway underlying the condition. The research, conducted by experts at the University of Pennsylvania, points to depleted serotonin levels as a key factor in the manifestation of certain long Covid symptoms, including memory problems and neurological and cognitive issues. This discovery has significant implications for the diagnosis and treatment of long Covid, a condition that presents in various forms and often eludes conventional diagnostic tools.
The study suggests that the reduction in serotonin levels may be triggered by residual viral remnants lingering in the gut. This revelation has the potential to open doors to innovative treatments, including medications designed to boost serotonin production. Additionally, the researchers propose that their outlined biological pathway could serve as a common link between various theories surrounding the causes of long Covid, such as the persistence of viral remnants, inflammation, increased blood clotting, and autonomic nervous system dysfunction.
 As Christoph Thaiss, a lead author of the study and an assistant professor of microbiology at the Perelman School of Medicine at the University of Pennsylvania, states, “All these different hypotheses might be connected through the serotonin pathway.” He also highlights the possibility that therapies targeting the serotonin pathway could benefit at least a subset of individuals with long Covid.
As Christoph Thaiss, a lead author of the study and an assistant professor of microbiology at the Perelman School of Medicine at the University of Pennsylvania, states, “All these different hypotheses might be connected through the serotonin pathway.” He also highlights the possibility that therapies targeting the serotonin pathway could benefit at least a subset of individuals with long Covid.
Akiko Iwasaki, an immunologist at Yale University, commends the study, describing it as “an excellent study that identifies lower levels of circulating serotonin as a mechanism for long Covid.” She notes that her team and colleagues at the Icahn School of Medicine at Mount Sinai have recently conducted a study that identified other biological changes associated with some cases of long Covid, including hormone cortisol levels. These findings suggest that there might be specific subtypes of long Covid or different biological markers at different stages of the condition.
The research involved the analysis of blood samples from 58 patients who had been experiencing long Covid symptoms for a duration ranging from three months to 22 months post-infection. These results were compared to blood samples from 30 individuals with no post-Covid symptoms and 60 patients in the early, acute stage of a coronavirus infection.
Maayan Levy, a lead author of the study and an assistant professor of microbiology at the Perelman School of Medicine, highlights that serotonin levels and other metabolites were altered immediately following a coronavirus infection, a pattern observed with other viral infections. However, in individuals with long Covid, serotonin was the only significant molecule that did not return to pre-infection levels.
The researchers delved deeper into their investigation by analyzing stool samples from some long Covid patients, where they discovered the presence of residual viral particles. Through a combination of patient data and studies on mice and miniature models of the human gut, where serotonin production primarily occurs, the team identified a potential pathway contributing to certain long Covid cases.
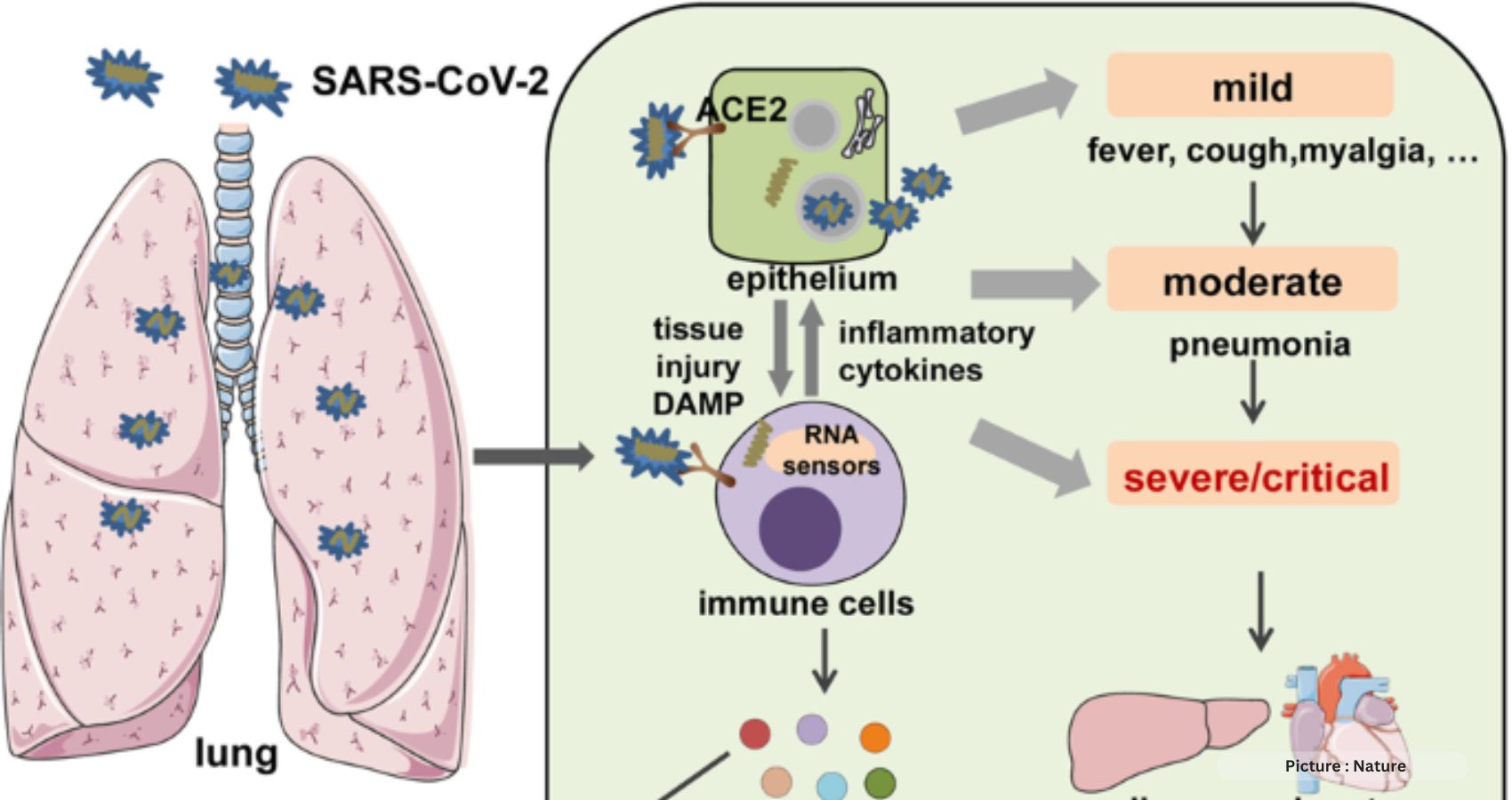
The proposed mechanism revolves around viral remnants prompting the immune system to produce interferons, which are proteins that fight infection. Interferons induce inflammation, reducing the body’s ability to absorb tryptophan, an amino acid crucial for serotonin production in the gut. Moreover, blood clots that can develop following a coronavirus infection may impair the circulation of serotonin in the body. Depleted serotonin levels are believed to disrupt the vagus nerve system, which transmits signals between the body and the brain. As serotonin plays a role in short-term memory, this disruption could potentially lead to the memory problems and cognitive issues often experienced by individuals with long Covid.
While the study presents a promising breakthrough, there are some caveats to consider. The sample size was relatively small, necessitating the confirmation of these findings through additional research. Moreover, participants in other long Covid studies, which included individuals with milder symptoms, did not consistently exhibit depleted serotonin levels. This variation might suggest that serotonin depletion occurs primarily in individuals with more severe and complex long Covid symptoms.
In the quest to identify biomarkers for long Covid, which are measurable biological changes that aid in diagnosing the condition, this study has put forth three potential indicators: the presence of viral remnants in stool, reduced serotonin levels, and elevated interferon levels. Most experts believe that there won’t be a single biomarker for the condition; instead, several indicators may emerge, varying based on the type of symptoms and other factors.
The need for effective long Covid treatments is substantial, and clinical trials testing various treatment approaches are currently underway. Dr. Levy and Dr. Thaiss have announced their intention to launch a clinical trial to evaluate fluoxetine, a selective serotonin reuptake inhibitor often marketed as Prozac, and potentially tryptophan. They hope that supplementing serotonin or preventing its degradation could help restore vagal signals and improve memory and cognition in individuals with long Covid. This research paves the way for novel diagnostic methods and potential therapies to address the multifaceted challenges of long Covid.